When a pain or pressure forms in your head, are you able to tell with certainty if it’s a headache or migraine – or potentially something more severe like a brain aneurysm or another underlying health condition?

It’s not always easy to tell. And much like the confusion people experience when identifying a cold or flu, differentiating between headaches, migraines and aneurysms can lead many people to incorrectly determine what they’re suffering from.
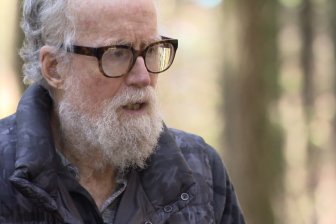
“When people talk about migraines for example, they often mistake them for just a headache,” said Dr. Ian Finkelstein, headache expert at the Toronto Headache and Pain Clinic in Toronto. “So migraines are not headaches and are, in fact, a neurological condition that is a disabling headache… Migraines are also significantly under-diagnosed in Canada and under-treated.”
READ MORE: Not just for wrinkles: How Botox is helping ease migraine pain
According to MigraineCanada.org, it’s estimated that 2.7-million Canadians (or 8.3 per cent of Canadians) are diagnosed with severe headaches.
And did you know that there are more than 200 types of headaches classified by the International Headache Society?
So how does one know if they’re experiencing a headache, migraine or aneurysm – and is there anything that can be done to prevent or treat such head pain?
What kind of pain is it?
- Buzz kill? Gen Z less interested in coffee than older Canadians, survey shows
- Naloxone-resistant street drug linked to 9 deaths in Eastern Canada seized in Alberta
- Bird flu risk to humans an ‘enormous concern,’ WHO says. Here’s what to know
- ‘She gets to be 10’: Ontario child’s heart donated to girl the same age
The symptoms of a headache, Finkelstein says, are straight forward. They are not debilitating, but they can cause enough discomfort that will slow people down. Usually, however, people are able to carry on with their days and don’t lose their ability to function.
Specifically, a headache’s symptoms typically include dull, aching head pain and a sensation of tightness or pressure across the forehead or on the sides and back of the head. People may also experience tenderness of the scalp, neck and shoulder muscles, the Mayo Clinic outlines.
Headaches are classified into two categories: episodic and chronic.
Episodic tension headaches can last anywhere from 30 minutes to a week. They usually happen less than 15 days a month for at least three months.
Chronic headaches can last for hours and may be continuous. If they occur 15 or more days in a month for at least three months, they’re often considered chronic.
Migraines, however, are far more painful, Finkelstein said.
“When migrainers develop a headache, it’s moderate to severe in nature, their function is disabled and they often experience other signs that typical headache patients don’t experience like nausea, vomiting, light and sounds sensitivity,” Finkelstein explains. “Migraines are primary headaches – in other words, there is no other underlying reason for the headaches.”
According to the Mayo Clinic, other symptoms of a migraine include a severe throbbing or pulsating pain (usually just on one side of the head). An aura may also occur before along with the migraine – like a flashing light, blind spots or tingling in the arm, leg or one side of the face.
“Patients with brain aneurysms are suffering from what we call secondary headaches,” Finkelstein said. “There is often some tell-tale signs that these patients may experience that may alert them or a physician that other testing is necessary.”
However, sometimes aneurysms can go unnoticed, Finkelstein warns. But one big symptom to look out for is called a “thunderclap headache.”
“They can leak and cause a severe on-set of a headache called a thunderclap headache,” he said. “Patients will often cough, sneeze or bear down when they’re having a bowel movement, for example, and develop a headache… Patients explain it as the worst headache they’ve ever had. That is often a sign that something else is going on that would be concerning with respect to a secondary headache, and those are the patients that ought to visit an emergency room right away.”
Aneurysms usually have to be detected through a brain imaging scan called an MRA, which is an MRi with an injected contrast dye. The dye is used to light up the blood vessels and alerts the doctor to a possible brain aneurysm.
Know the triggers
Triggers for headaches and migraines can differ depending on the person.
Simple triggers for headaches and migraines can include poor posture, coffee withdrawal, skipping meals, dehydration, intense exercising, heat and stress.
READ MORE: AHS offers free workshop for those prone to weather-related headaches and migraines
Other common triggers include a change in barometric pressure, certain foods, a change in sleep patterns and women’s menstrual period.
Aneurysms are a different story, Finkelstein said.
“I don’t think there is an absolute trigger for headaches caused by an aneurysm,” he says. “I think that if patients develop a headache as a result from coughing, sneezing or some type of manoeuvre – that may be a warning sign. It might not actually trigger something, but it may be a warning sign that something else is going on and they should seek medical attention.”
How to treat
Simple headaches can be treated with ibuprofen, acetaminophen and Aspirin, according to the Mayo Clinic.
Anti-inflammatories like ibuprofen can also be helpful for migraine sufferers.
Sometimes the pain may be too overwhelming for migraine patients, in which case they often confine themselves to dark, quiet rooms to rest, Finkelstein said.
Other aids include hot or cold compresses to the head and neck, massage and small amounts of caffeine. A patient may also be prescribed other medications, like sumatriptan or zolmitriptan by their doctor is it’s a persistent problem, the Mayo Clinic says.
When to seek medical attention
While migraines are common, sometimes they may signal another underlying issue, Finkelstein said.
“Anytime a patient comes in with a headache, the physician needs to go through a comprehensive history to rule out secondary-causes of headaches to make sure that something else isn’t going on like an aneurysm or tumour in the brain, an infection in the brain or changes in the cerebral spinal fluid,” he said. “These are all secondary causes of headaches that need to be ruled out, but they can be ruled out by doing a proper medical history.”
And once those second causes are ruled out, that’s when doctors must distinguish which primary-type of headache the patient has. For the majority of patients, it will be diagnosed as migraines, Finkelstein said.
With brain aneurysms, however, medical intervention is needed.
“If there is an aneurysm that’s leaking and causing a headache then a neurosurgical consultation is needed and it obviously needs to be treated within a hospital,” Finkelstein said.



Comments