In the wake of B.C.’s provincial health officer labeling the spike in overdoses in the province a “public health emergency,” the Interior Health Authority is beefing up its overdose response.

Seven emergency departments in the heath authority, including the emergency departments in Vernon and Kelowna, have already put into effect a new system to track overdoses and have begun distributing naloxone kits through the Take Home Naloxone program. The health authority says “within the next two months” it plans to expand the programs to all emergency departments in the region.
Read More: Spike in Okanagan drug overdose deaths, latest numbers from B.C. Coroners
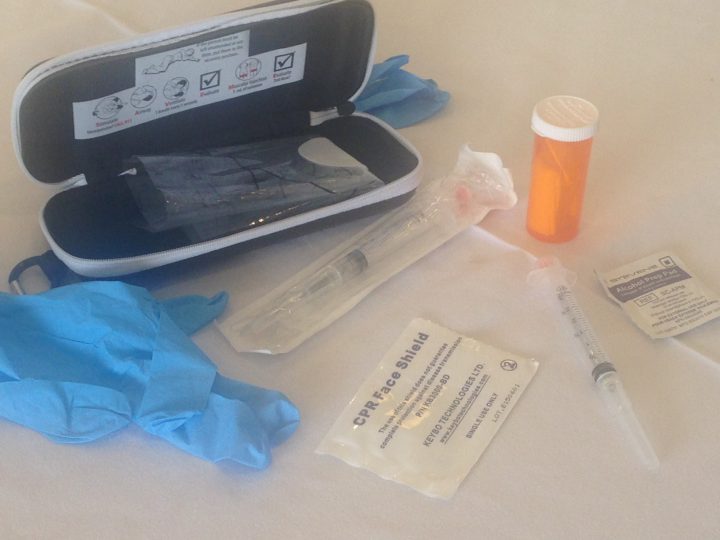
With the Take Home Naloxone program those deemed “at risk of an overdose” can pick up a potentially life-saving naloxone kit and receive training on how to use it.

Get weekly health news
“Naloxone is an injectable drug that can reverse (stop) an opioid overdose – in the event of an overdose, naloxone restores breathing within 2-5 minutes, which offers the opportunity to save a life and reduce harm while waiting for help to arrive,” the Interior Health Authority explains in a media release.
The second initiative, already in place in Vernon and Kelowna, that is being implemented across the health authority is a more formal system to track overdoses. Staff will fill out a detailed form about every overdose that comes into the emergency department.
“The enhanced surveillance will allow us to identify where risks are arising and will enable us to take proactive action to warn and protect people who are at risk,” wrote spokesperson Lesley Coates in an emailed statement.
The move follows an April announcement in which provincial health officer Dr. Perry Kendall called the high level of overdoses plaguing B.C. a “public health emergency” and talked about collecting more information on the problem.
Read More: Little if any heroin left in Vancouver, all fentanyl: drug advocates
“Health authorities have consistently asked for more data that will help inform responses and prevent future overdoses,” said Kendall in April. “Over the next few weeks, I’ll work with medical health officers, health authorities, emergency room staff, paramedics and other first responders and the BC Coroners Service to determine how best to collect and share the data.”
In April, the province said if nothing was done to stem the tide of overdoses, the province was on track to record 600 to 800 overdose fatalities in 2016.







Comments