London Health Sciences Centre (LHSC) and London InterCommunity Health Centre (LIHC) have formed a partnership to help marginalized women receive vital prenatal care.

The women that the obstetrics clinic are trying to reach struggle with accessing healthcare in hospitals or other locations that require a commute.
“A lot of us have been serving the marginalized community for 34 years,” said Greg Nash, Director of Program Development and Complex Urban Health. “Part of that experience is women who are pregnant, who might be street involved, experience precarious housing, mental health issues, chronic disease and substance use disorders.”
Nash and his team at LIHC work alongside two OB-GYN’s and one Family Medical Obstetrician from LHSC, Dr. Laura Lyons, to provide care for women who are pregnant, up until six weeks after their birth. This timeline is case-dependent and allows for longer follow-up care if need be.
“Because of their circumstances, health care they experienced in the past sometimes isn’t good or doesn’t produce positive health outcomes, so the trust they have in the health-care system is reduced,” said Nash. “This partnership (between LHSC and LIHC) evolved because our community workers and clinicians identified this was problematic.”
The commitment of the team of OB-GYN’s extends to their patients’ labour and delivery as well.
“Part of our plan is to support these folks with Dr. Easterbrook, Dr. Hudson and Dr. Lyons to visit the hospital with them,” said Nash. “Actually go with them and do that introduction to help build that trust, to help build that positive experience, so that can continue.”

Get daily National news
Dr. Lyons is a key member in the creation of the new clinic and will be helping the patients on site on a rotating schedule. When Lyons initially reevaluated the barriers that women were facing, causing them to miss appointments, she realized the health-care system wasn’t providing the best care they could.
“This is why we decided to bring our services to where the women feel safe. LIHC is a place they have been coming to, prior to becoming pregnant, for health care.”
The location will be the primary change in that patients don’t need to travel to be seen at the clinic, as well as the quality of care.
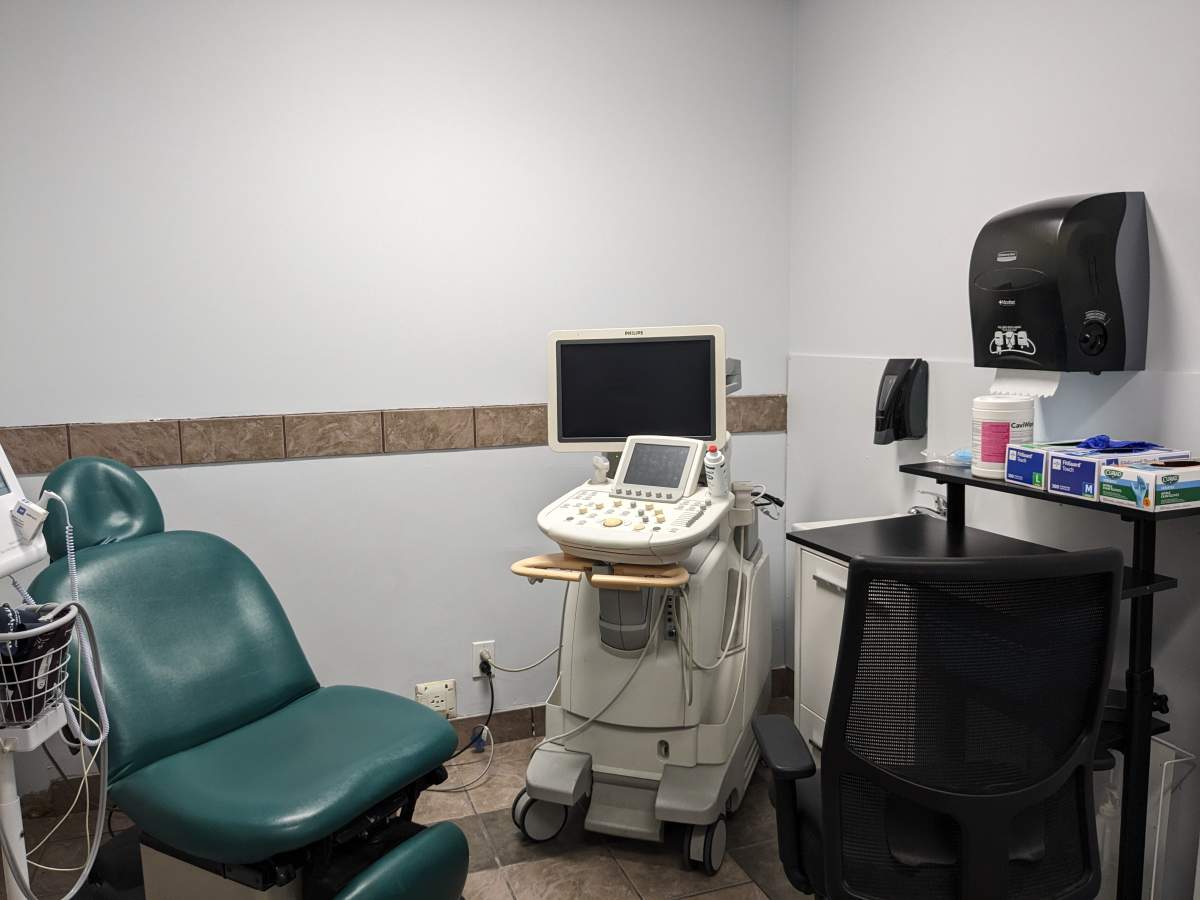
“This is going to be one stop shopping,” said Lyons. “they’re going to be able to get their ultrasounds, their blood work and their physician care here.”
The clinic also has space for patients to do their laundry, bring in their companion animals or have showers, and offers support for housing, food security and mental health.
“This care is patient-centred. We’re identifying what the patient needs and how health care should be delivered,” said Lyons.
The clinic runs biweekly on Wednesdays, and has been open since Jan. 10, 2024. Since the establishment of the clinic, they have received two ultrasound machines that LHSC would otherwise have put into storage, according to Brad Campbell, corporate hospital administrative executive at LHSC.
When asked if the ultrasound machines were the most noteworthy investment, Campbell instead referred to the commitment from physician partners in leadership roles to come to be at the clinic. “There was no hesitation.”














Comments