Editor’s note: Due to the changes in Alberta that severely limit who can be tested for COVID-19 by Alberta Health Services, our coverage will no longer prioritize daily case counts, instead focusing on hospitalization numbers. We will continue to publish daily case counts on our website with a note that the lab-confirmed cases do not reflect all cases in the community, and monitor those counts for trends that merit further questions and analysis. In addition, the dates in the photo captions have been corrected to reflect the date on which the wastewater samples were collected. We regret the error.

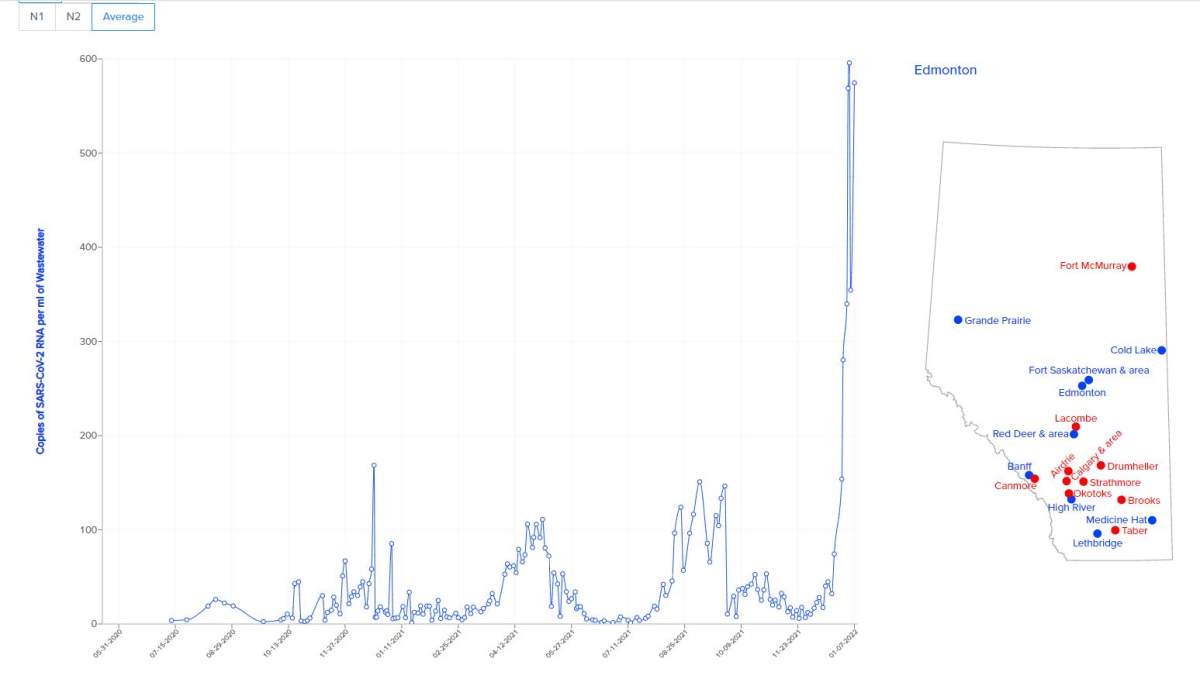
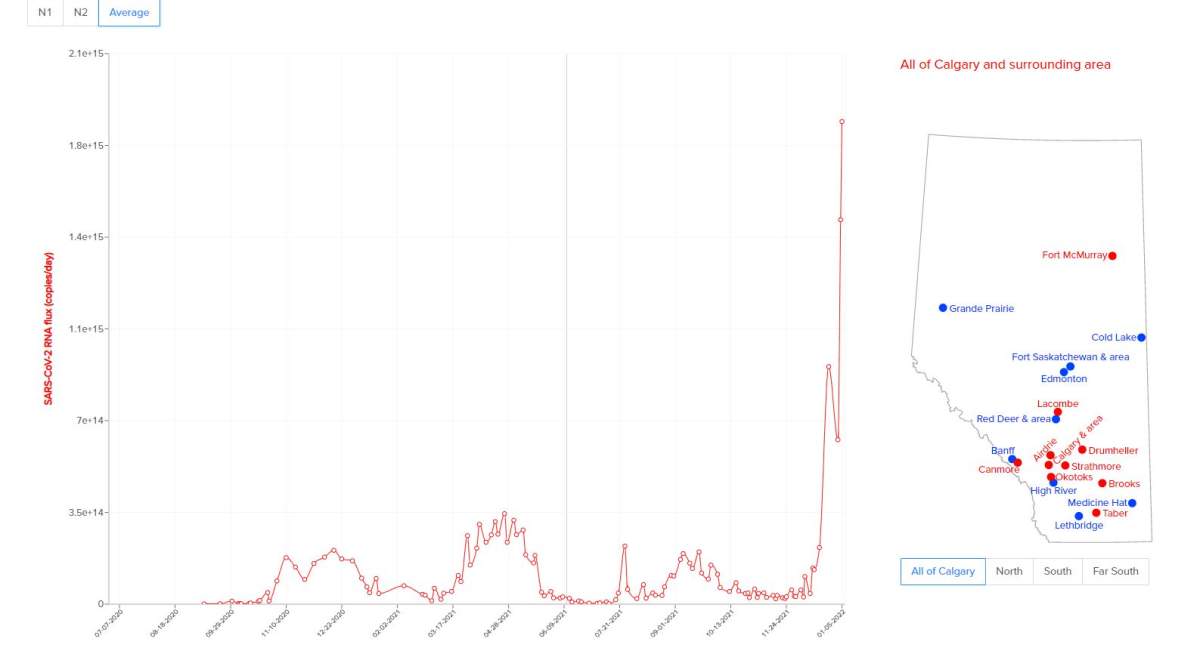
Wastewater sampling in Alberta shows levels of COVID-19 infection that the province has not seen since the pandemic began.
The new data comes as hospitalizations due to COVID-19 increased to 708 Tuesday, up from 635 on Monday. There are now 80 people in the ICU being treated for COVID-19, up from 72 people on Monday.
Alberta recorded eight additional deaths in the last 24 hours, bringing the province’s death toll to 3,352. (See Tuesday’s full COVID-19 data below).
Researchers at the University of Alberta and University of Calgary have been monitoring wastewater for COVID-19 in Alberta for nearly two years, tracking the amount of virus in communities at any given time.
The process monitors virus that is shed in the stool of infected individuals six days before cases are clinically diagnosed.
“What’s really important about wastewater is it’s conclusive and comprehensive. (It) includes all members of society, even those that are marginalized, and it includes all individuals whether they have symptoms or not and whether they get tested or not,” said Michael Parkins, an infectious disease physician and associate professor in the department of medicine at the U of C’s Cumming School of Medicine.
“It’s a perfect tool for monitoring COVID-19 on a community level and to be used in conjunction with clinical testing.”
Samples are collected three times per week. Parkins said all major towns and cities across Alberta have seen a “steep increase” recently in COVID-19 case burden, driven by the highly transmissible Omicron variant.

“We’ve seen levels now eight or nine or 10 times higher than we’ve seen in any other COVID-19 wave,” he explained Tuesday, adding this means that COVID-19 exists at a higher level than ever before in Alberta.
“SARS-CoV-2 values in wastewater are particularly higher… than we’ve ever seen before and we see that throughout communities in Alberta right now.”
Parkins said December saw the “near complete displacement” of the Delta variant with Omicron.
“In the beginning of December it was 100 per cent Delta and by mid-December in our large cities, 50 per cent was already Omicron,” he said. “As of last week we’d seen that across the board in all but two small communities, Omicron was 90 per cent or more of the wastewater signal for SARS-CoV-2 RNA.”

Get weekly health news
The physician went on to say that “what is somewhat heartening is that the cases being admitted to hospital and certainly the cases being admitted to ICU are much, much fewer than what we’ve seen in prior pandemic waves, telling us that again, the virus is evolving.”
The province has put an increased reliance on wastewater testing in recent weeks, after limiting who in Alberta is eligible for PCR COVID-19 testing.
Alberta’s chief medical officer of health Dr. Deena Hinshaw said Monday that cases brought on by the Omicron variant have swamped testing — people wanting a PCR lab test need to book days in advance and are waiting up to two days to get results back.
Starting immediately, she said only high-risk cases are eligible for PCR tests, including continuing care residents and front-line health-care workers, in order to speed up processing.
“We’re having significant challenges in getting timely access to testing and results for people who really need it to manage their clinical scenarios,” Hinshaw said.
Before that, those cases had been the priority for testing but those who did not have access to rapid tests could still book a PCR test.
“We’re working hard to make rapid tests more widely available,” said Hinshaw.

Lorian Hardcastle, an associate professor in the faculty of law at the Cumming School of Medicine, said the shift in the testing policy has added an extra layer of stress for Albertan unable to access rapid testing.
She pointed specifically to those whose employers are asking for proof of positive test results, those who are dealing with long COVID and those worried about worker’s compensation.
“The publicly funded rapid test kits are gone from pharmacies and the paid ones are there, but that creates a two-tiered system where some can pay, some can’t. And furthermore, if people are symptomatic they’re not supposed to be at pharmacies getting rapid tests, they’re supposed to be at home isolating. So it’s quite a difficult situation for people,” she said.
“When you take away the ability for people to get tested, then people don’t know if they’re positive or not, or don’t know what they should be doing from a safety perspective, or their employer is asking for a test and they don’t whether they should follow the rules or just go to the store and not isolate and get a test — that puts a lot of pressure on individuals.”
She believes the province needs to keep communicating to employers, worker’s compensation personnel and private insurers to reinforce the message not to ask employees for proof of positive test results.
“The average Albertan is having to fumble their way through this and be stressed about how to solve this problem on their own.”

On Monday, Hinshaw had the following message on the matter:
“I want to emphasize that I urge employers and organizations to not require proof of a positive COVID-19 result to support sick leave requests right now. With our test positivity currently at 40 per cent, anyone who has COVID symptoms almost certainly has COVID and should just be staying home.”
Dr. Anmol Kapoor, founder of CardiAI Labs, said the testing changes will lead to a spike in demand at private clinics.
“We can do many more tests, we have capacity to do thousands of more testing a day if we have to,” Kapoor said.
Some private clinicians question why they’re not being called upon to increase testing capacity.
“We are two years into the pandemic. We shouldn’t be struggling for tests. We are a rich country with resources and should be able to afford multiple tests for multiple people again and again,” Kapoor said.
“Why can’t government agencies reach out to private companies and provide them the coverage? Why can’t they create billing codes for tests and patients can get tests done? I truly feel we failed our patients because of policy paralysis. We should provide care to patients whether they can afford the test or not afford the test.”
The Alberta government has not yet responded to a request for comment regarding the use of private companies to help with testing capacity.
Tuesday's COVID-19 data
Alberta reported 4,704 lab-confirmed cases of COVID-19 on Tuesday, from about 12,200 tests.
The province’s positivity rate was about 38.5 per cent.
There are now 58,613 lab-confirmed, reported active cases of COVID-19 in Alberta.
Because of the limited testing capacity in Alberta, health officials have said this is likely just a fraction of the total number of cases in the province right now.
“We should assume that at minimum we’re seeing about 10 times or more the number of cases that we’re diagnosing through PCR (tests),” Hinshaw said Monday.
With files from The Canadian Press.











Comments
Want to discuss? Please read our Commenting Policy first.