In a world-first, researchers out of Lawson Health Research Institute and Western University in London, Ont., have profiled the immune system’s response to COVID-19 and identified six molecules they believe can be used as therapeutic targets to treat the virus.

Some early reports from scientists and physicians suggested that the novel coronavirus can cause a cytokine storm in some patients, which is when the immune system goes dangerously overboard in responding to an infection.
“That inflammation that occurs is important for ridding the body of the virus, but the flip-side of that is if it’s exaggerated, the inflammation can actually start to destroy your own tissues,” lead researcher Dr. Douglas Fraser explained on The Craig Needles Show on Thursday morning.
“What’s been happening is in a rush to find some interventions, people have been speculating, ‘maybe it’s this cytokine, maybe it’s this cytokine, maybe it’s that one.’ We took a little bit of a different approach.”

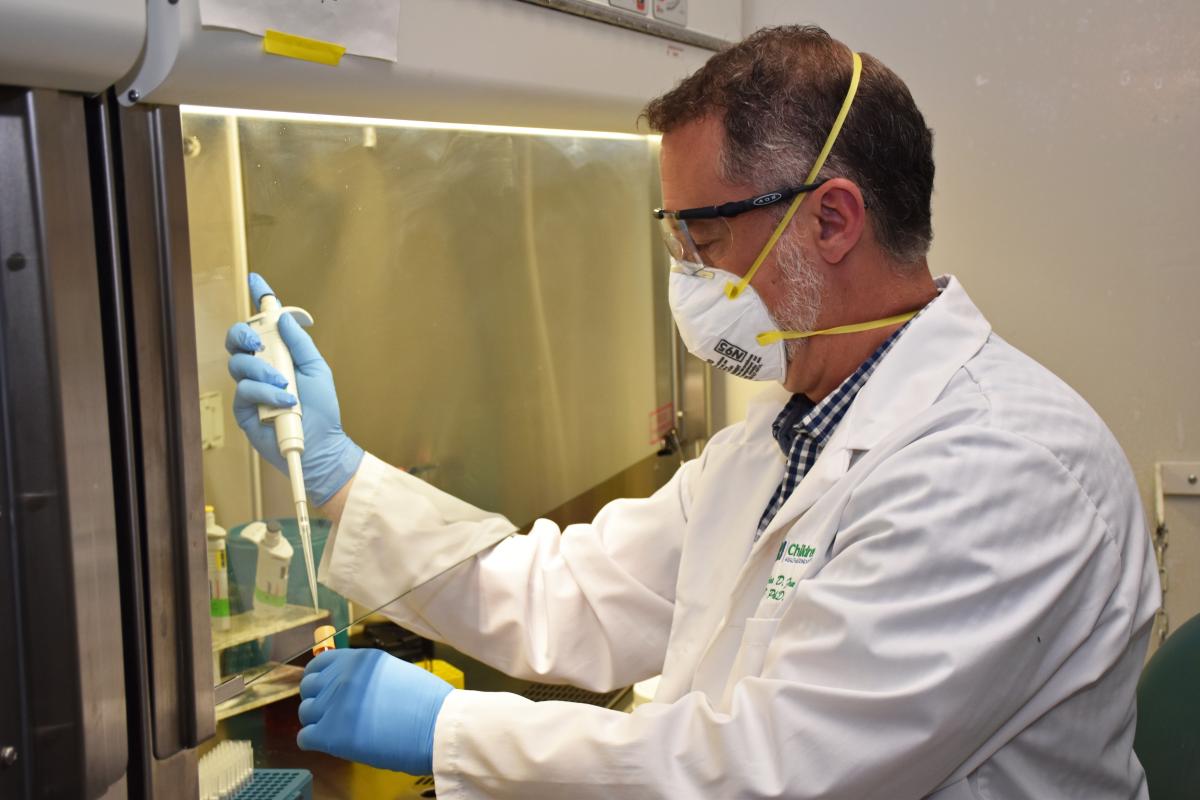
A study was launched in March and published this week in Critical Care Explorations looking “at 57 of the most common and implicated cytokines that are floating around in your blood.” Researchers found six that were “critical for the COVID-19 patients.”
“They were not only dramatically elevated relative to other infections in sick people but they were also persistently elevated — they didn’t come back down like many of the cytokines do.”
The molecules are tumor necrosis factor, granzyme B, heat shock protein 70, interleukin-18, interferon-gamma-inducible protein 10 and elastase 2. Heat shock protein 70, in particular, was “strongly associated with an increased risk of death when measured in the blood early during the illness.”

Get weekly health news
Fraser says this data allowed them to come up with therapeutic targets and the next step is to test drugs that can block the harmful effects of the molecules while still letting the immune system fight the virus.
“That’s the first process we want to go after and we’ve got a clinical trial being planned with effective inhibitors that have been used previously against these enzymes in clinical trials, so we’ll try that.”
Researchers studied blood samples from 30 participants: 10 COVID-19 patients, 10 patients with other infections admitted to the intensive care unit at London Health Sciences Centre (LHSC), and 10 healthy participants as the control group.
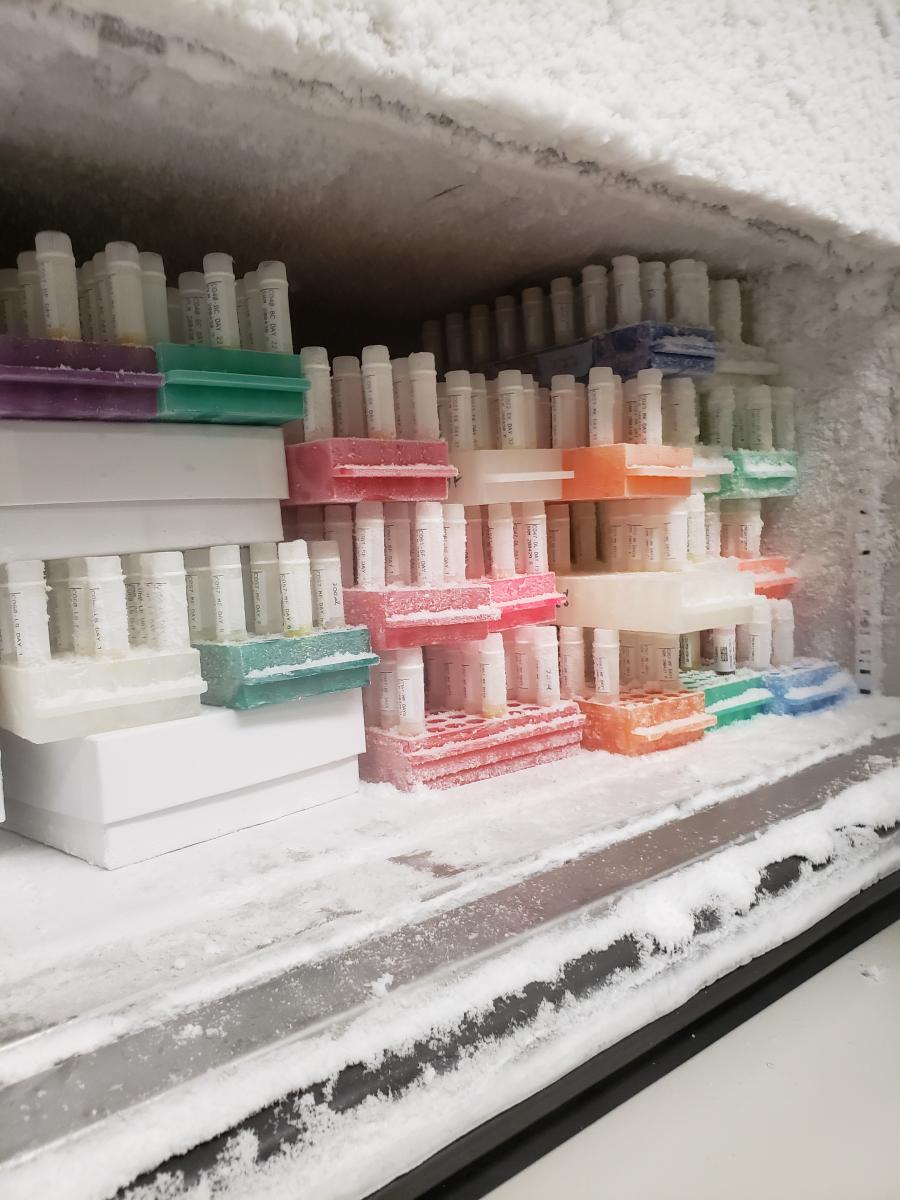
“We saw our first patient in mid-March. To go from mid-March to three months later to have collected 13,000 vials of human specimens, which is what we have in our freezer,” said Fraser, “to do that in three months and be able to fully profile, characterize the immune response… is really remarkable.”
Fraser noted that the specimens are also shared with “the vaccination groups, with the immunoglobulin groups as well, and our data is being shared with other scientists around the world.”
Lawson Health Research Institute says the study was made possible with donor support to London Health Sciences Foundation as well as additional funding from Lawson, Western, and the AMOSO Innovation Fund.















Comments