WATCH ABOVE: Ebola been around for nearly 40 years but never has there been a known case in Canada. As Angie Seth reports, we should know within 24 hours if that “virus free” status stands.

TORONTO – As doctors monitor a patient being tested for Ebola, Ontario’s health officials say they’re confident the province is prepared and ready to contain any potential cases of the virus.
Doctors at a Brampton, Ont., hospital are determining if the patient has Ebola. The patient is showing flu-like symptoms similar to the deadly virus and recently travelled to Nigeria, one of the four West African nations hit by the outbreak.
Blood samples from the patient were sent Friday to Winnipeg’s National Microbiology Laboratory for testing. Results from the lab are expected within the next 24 hours according to a statement from province’s health ministry.
READ MORE: Ontario hospital treating patient for Ebola-like symptoms

Get weekly health news
Right now, there are no confirmed cases of Ebola in Canada and experts say the risk is low.
Hoskins says that initial signs and symptoms of Ebola are similar to other diseases, such as malaria and pneumonia.
Ebola haemorrhagic fever (EHF) is one of the most notorious viruses known to mankind and its marked by the sudden onset of intense weakness, fever, muscle pain, sore throat and headaches.
Victims’ symptoms include diarrhea, vomiting, multi-system organ failure, and internal and external bleeding. In its final stages, some patients bleed from their eyes, nose, ears, mouth or rectum. But at the onset, it typically presents as a respiratory illness.
READ MORE: What the WHO’s international health emergency declaration means
Dr. Graham Pollett, the province’s chief medical officer, says that hospitals are bracing for a potential case, but that our health care system is built on “sophisticated infection control systems” and protocol to protect frontline health care workers.
For now, the Brampton patient is in isolation as a precaution. Brampton Civic Hospital also heightened its infection-control measures.
After months of battling the largest and longest outbreak of Ebola ever recorded, the World Health Organization (WHO) declared the epidemic an international public health emergency Friday.
The global authority is calling on health officials around the world to take on extraordinary measures in an attempt to stop the spread of Ebola.
“Countries affected to date simply do not have the capacity to manage an outbreak of this size and complexity on their own,” WHO chief, Dr. Margaret Chan, said at a news conference in Geneva.
READ MORE: Why health officials say the Ebola epidemic won’t spread into Canada
Dr. Michael Gardam, the director of infection prevention and control atUniversity Health Network, is resolute in ensuring the public: Canada’s health care system has strong protocols in place and public health officials learned their lessons from SARS in 2003.
Post-SARS, protocol for nurses, doctors and paramedics changed dramatically and surveillance is now in place brokering intelligence on rising diseases that could pose a threat.
Patients are now screened for a fever, cough or trouble breathing. They’re asked a critical, telling question: have they recently returned from another country? Frontline health care workers assessing them don masks, gowns, gloves and any other equipment that acts as a safeguard.
READ MORE: SARS 10 years later – how has the health care system changed?
Hospitals have better ventilation, single rooms, and plexiglass walls act as a barrier between emergency room front desks and sick patients.
There’s also compliance to advice doled out by health officials.
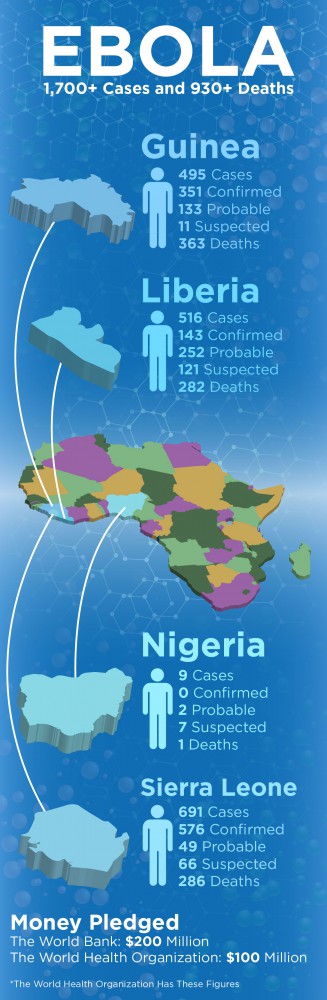
More than 1,700 people have been sickened in the current outbreak in four countries – Nigeria, Liberia, Sierra Leone and Guinea. Nearly 1,000 people have died, according to WHO estimates.
carmen.chai@globalnews.ca
Follow @Carmen_Chai







Comments