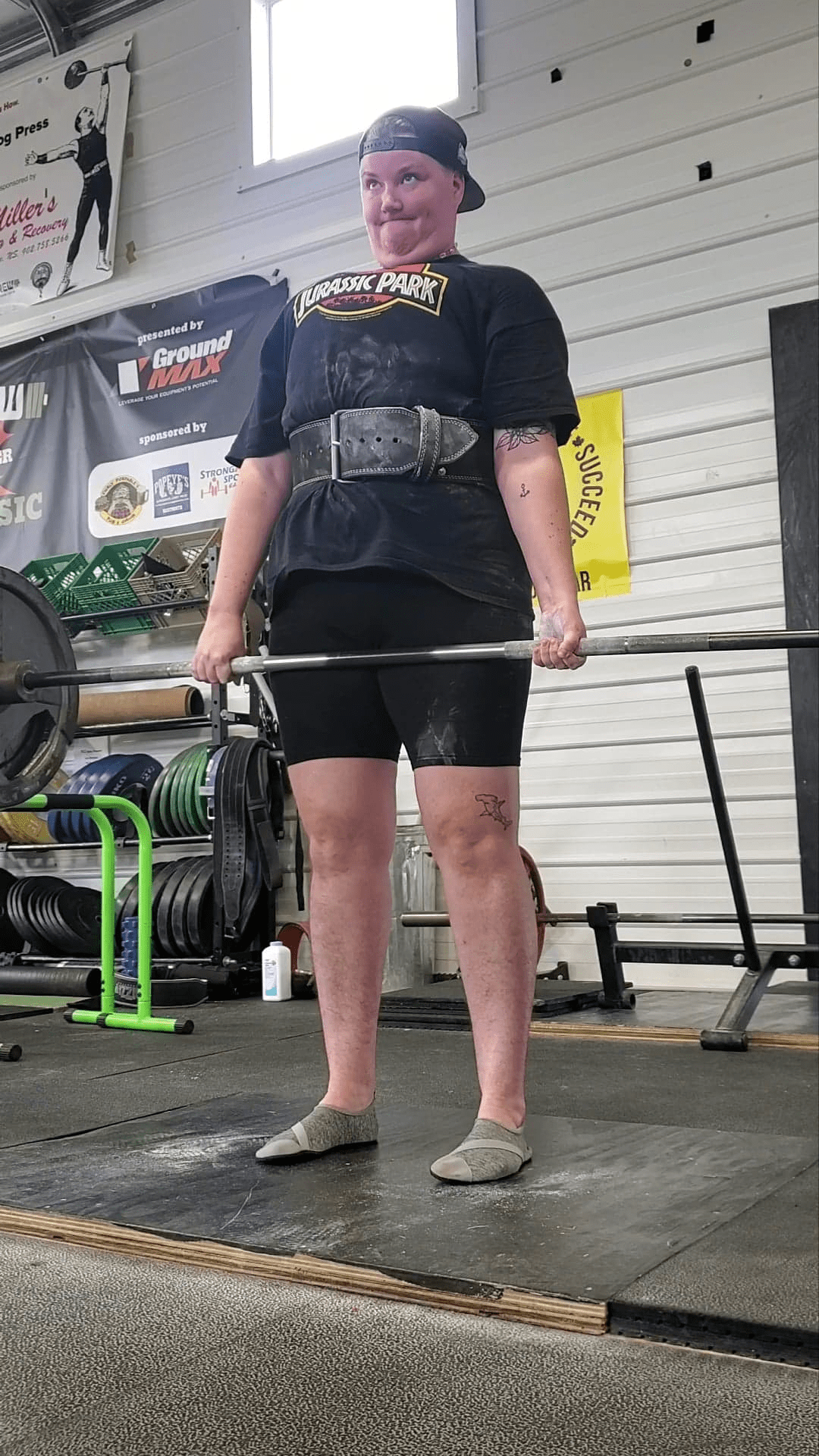
It has been a long road to self-discovery for Felix Vandergrift.

After years of battling an eating disorder, body dysmorphia, substance abuse and mental health issues, Vandergrift says things came to a head at 29 years old, when they were admitted to hospital.
“I legitimately have a nervous break. My anxiety gets so bad that I actually end up in the hospital because I don’t know what else to do — I’m just not feeling any better,” said Vandergrift, now 33.
“I’m very lucky to have my family and my partner and my friends support me, and a lot of chosen family support me during that time, or else I wouldn’t be here.”
They began unpacking their issues, and through that came clarity, Vandergrift said. They began medically transitioning in March 2021 and added their name to the list for a gender-affirming top surgery through MSI.
“As soon as I started on that path, I knew it wasn’t going to be easy, but it was worth it,” they said.
So when Vandergrift learned that the only doctor performing gender-affirming top surgeries through MSI had decided to stop providing the service under provincial coverage, it came as a shock, they said.

However, they decided to go ahead and book a consult for March 2023, saying they would figure out the financial details later.
“So we go through the process of booking the consult and she asks for my height and weight, and I immediately am just like, ‘I know what’s coming,’” said Vandergrift.
“She immediately says your BMI (body mass index) is too high, you’re going to need to lose weight before your consult.”
Vandergrift said as someone who’s been dealing with disordered eating and body image issues for years, it came as a massive blow.

Get weekly health news
“I’ve just in the last four or five years done a lot of therapy outside of my own personal gender issues to work on that,” they said.
“And one of the requirements for getting gender-assignment surgery is having your mental and medical issues under control, so now they’re telling me I need to lose a significant amount of weight in order to get the surgery.
“She says, ‘But it’s okay, you’ve got lots of time, you’ve got eight or nine months to lose the weight.’ And I said, ‘Well, I’m not going to.’” And she said, ‘Well, then we can’t book your consult.’ So I was even denied a consult based on my BMI.”
Province reviewing policy
When asked Thursday whether the province would consider scrapping BMI as a deciding factor for gender-affirming surgeries, Nova Scotia Health Minister Michelle Thompson said it’s something they will look into as they are currently in the process of reviewing their gender-affirming care policy.
“As we review that policy and we hear from people directly that will probably come up in terms of what some of the barriers are,” said Thompson.
She said there are issues around risk that need to be considered, and historically BMI is one of the tools used to assess risk associated with surgery.
“We will continue to hear from people directly and understand how the current policy impacts their ability to access care and see where we can adapt and implement things that would make it easier, but always looking at safety and quality of care first.”
Opposition critic Lisa Lachance, the first gender non-conforming person in the provincial legislature, said with Nova Scotia having the greatest proportion of trans and gender diverse people compared to any other province, the government needs to do better.
“We weren’t good enough anyway and we’re about to lose significant ground, so I think it’s really important to think about making these changes quickly so we can sort of re-orientate ourselves and make sure we’re providing the best care in Canada,” said Lachance, the MLA for Halifax Citadel-Sable Island.
They introduced a private members bill last month calling for the establishment of an independent, ministerial advisory committee on gender-affirming care.
“To put in place something that means that we’re constantly looking at how things are evolving, what’s happening in the province and what we should be doing,” said Lachance, adding it’s important to have “ongoing accountability to the community.”
Current care policy not working: Vandergrift
Vandergrift said the current gender-affirming care policy makes them “very angry.”
“It’s overly burdensome, it’s overly onerous, it’s overly complicated,” says Vandergrift.
“There’s this constant need to prove you’re trans, there’s a constant need to prove you have dysphoria. And all I can say to that is I really didn’t know I was trans until I started experiencing euphoria, and I started experiencing joy.”
Vandergrift said it’s been nearly one year into their medical transition and they’re already considering decreasing their anxiety medication.
“My anxiety and depression have not gone away, but they’re so much more manageable now that I feel like me,” they said.
“People that can’t access that care, it’s everything. And we’re going to lose people in an already vulnerable and marginalized community because they’re going to fall into the same issues that I had.
“That is dangerous. It’s not an over-exaggeration. It’s not dramatic, it is real.”









Comments