Experts think it will get worse before it gets better. It’s also triggered a team of local researchers to do a deep dive into what the opioid crisis looks like and what it means for those living in Saskatoon.

Between May and July of this year, 24 respondents were interviewed by the team – who provided key perspectives on the crisis in the community.
A group of stakeholders, who have been on the frontline, were brought together on Monday as part of a forum in an attempt to make sense of the crisis.
“How can we expect the public, policymakers, the health care sector or whoever is responding to this, if we don’t really understand what is going on and have a community-wide approach to this,” said Dr. Peter Butt, an addictions specialist with the Saskatchewan Health Authority and co-investigator of the study.
In addition to the interviews, the team from the University of Saskatchewan gathered data and drafted a discussion paper in order to formulate ways to respond to deadly drugs like fentanyl.
Some of the common themes that emerged were improving and expanding pain management programs in the province, increasing funding, improving education of professionals and the public as well as improving social determinants of health.
“We know what the solutions are, it’s just that we don’t always have access to those solutions,” said Dr. Wendy Gore-Hickman who now works as a recovery advocate.
Gore-Hickman said from her experience, those who need the help often don’t get it when they need it the most.

Get weekly health news
“I had one die on Oct. 5, he was waiting for a bed in Saskatchewan in one of our addiction centres and the wait list was six weeks,” Gore-Hickman said.
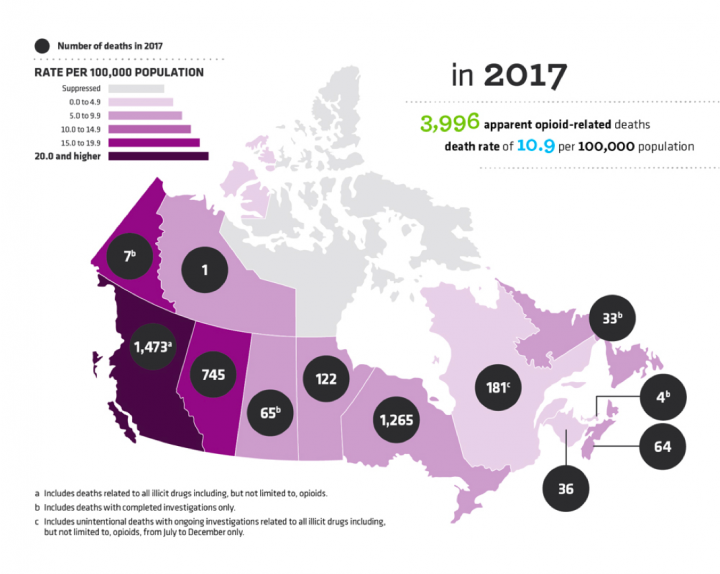
Based on the numbers above, it appears Saskatchewan’s crisis is not as dire as British Columbia’s but experts say even one death is too many. The figures are also raw statistics which means when it comes to deaths from illicit drugs, Saskatchewan’s rates are high on a per capita basis.
Saskatchewan also has some of the highest opioid poisoning hospitalization rates in the country and since 2015 there have been 54 fentanyl-related deaths. Marie Agioritis’ son Kelly Best was one of them after he took a green tablet and died.
“Talking to parents all the time, the questions from them are always the same ones I had – ‘What do I do? Where do I get help? Where do I go?'” Agioritis said.
“I didn’t know where to go and here today, I’m hearing where we can start to go.”
Dr. Barb Fornssler, with the University of Saskatchewan School of Public Health, underscored the need for change saying substance use impacts the entire community not just users and their families.
“In terms of economics, health care, crime rates and things like that – substance use does impact us all.”
The next step is finalizing the report, Consolidating Perspectives on the Nature of Saskatoon’s Evolving Opioid Crisis, and giving it to stakeholders, the Saskatchewan Health Authority and government officials.
“I think everyone has a stake in this, if they have this kind of information hopefully it will help make their response more informed and more targeted – so it’s more effective,” Butt added.



Comments