They are two different tests often conducted during the same medical visit to a family doctor: a Pap test for cervical cancer, and a test for a sexually transmitted infection (STI). Now that link could be putting patients at risk.

For years female patients would have a screening test for early signs of cervical cancer, known as a Pap test, often having it yearly. In 2012, Ontario introduced new guidelines recommending delaying screening until the age of 21 and saying women should have the Pap test less frequently. This guideline change is consistent with other provinces and the United States.
Since the guideline change, the number of girls and women receiving the Pap test yearly declined by 60 per cent – the unintended consequence was that the rates of screening for sexually transmitted infections (STIs) have plummeted, according to a new study.
“What was surprising and unintentional was that there was also a 50 per cent decrease in chlamydia and gonorrhea screenings subsequent to the updated guidelines,” Tali Bogler, a family physician at St. Michael’s Hospital told Global News.
According to the study’s authors, the Pap test and screening for STIs are linked because when female patients have a Pap test, it provides the opportunity for the patient and doctor to speak about STIs and perform the separate and different STI swab, urine or blood tests.
“Historically, we know that Pap tests and STI screening are linked because they’re often performed at the same time,” Bogler said.
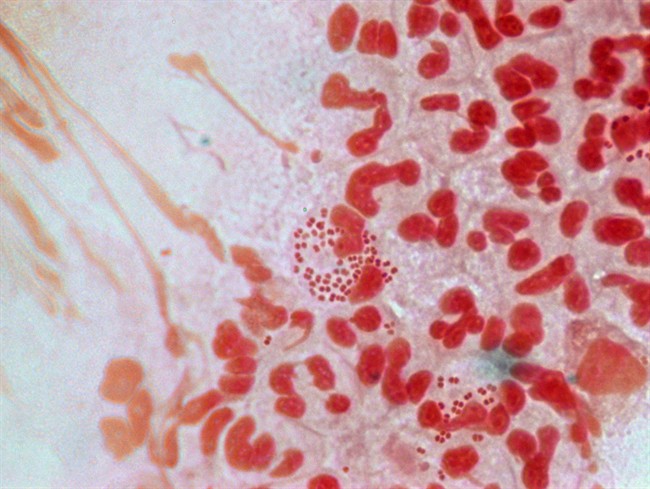
Gonorrhea and chlamydia are the two most common STIs in women aged 15 to 24 – often there are no symptoms. Over the past 10 years, chlamydia cases have risen by 72 percent and gonorrhea rates by 53 per cent, according to Public Health Agency of Canada.
The study authors also found that under the new Pap test cervical cancer guidelines, girls and women are less likely to be screened for syphilis, hepatitis C and HIV. The results were published in Canadian Family Physician.
Health consequences if not tested for STIs
“There are consequences to STIs if they’re not treated, and a lot of the time women are not symptomatic. The majority of the time with gonorrhea and chlamydia you’re not symptomatic so women are not being tested,” Bogler told Global News.
“If you’re not treated you can eventually have pelvic inflammatory disease, and that can lead to ectopic pregnancies and infertility and chronic pelvic pain, you know there’s serious consequences to that.”
In the United States, a different study from the Department of Family Medicine at the University of Michigan also showed a decline in the screening of STIs because of the cervical cancer screening change.
That study also showed a 50 per cent decrease in screening for chlamydia, after the guideline change. The results were published in the Annals of Family Medicine.
READ MORE: University of Windsor attempts to set record for most STI tests in one day
The Canadian authors urge that the two tests need to be uncoupled and there needs to be other options for patients.
“So I think family physicians really need to be aware of this risk, especially in younger women less than 21 who are at high risk of STIs,” said Bogler. “I think we need to move towards newer interventions to screen for STIs such as urine based sampling or self-administered swabs and to really think of innovative ways to screen at risk women”
- Buzz kill? Gen Z less interested in coffee than older Canadians, survey shows
- ‘She gets to be 10’: Ontario child’s heart donated to girl the same age
- Bird flu risk to humans an ‘enormous concern,’ WHO says. Here’s what to know
- Canada updating sperm donor screening criteria for men who have sex with men



Comments