TORONTO — Last month, Vancouver’s St. Paul’s Hospital took a step that not long ago would’ve been unthinkable: It closed its HIV/AIDS ward.

It wasn’t getting new patients.
British Columbia has become a global success story in combatting HIV/AIDS thanks to a made-in-Canada strategy that’s being adopted around the world – just not in Canada.
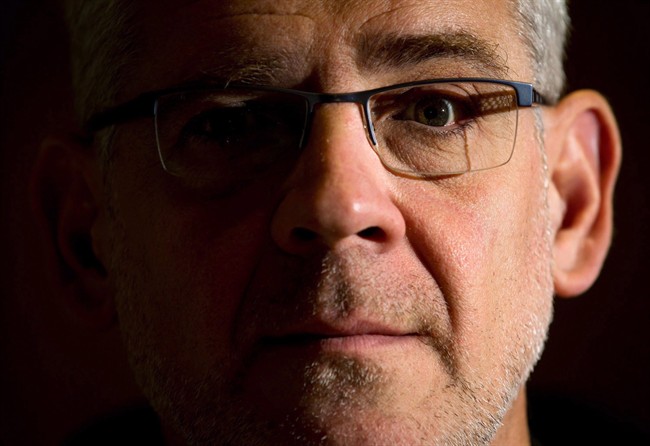
And the man behind this therapy doesn’t get it.
“We have worked very hard to convince jurisdictions across the country to embrace treatment as prevention. While we have made significant progress around the world and in global agencies, Canada remains reluctant to put forward a national policy,” Dr. Julio Montaner, the director of the B.C. Centre for Excellence in HIV/AIDS, told Global News.
READ MORE: HIV 30 years later: Experts mark milestones in treatment advances
Montaner has become internationally recognized for his HIV treatments — namely, highly active antiretroviral therapy, or HAART.
It’s a cocktail of three drugs taken daily first implemented in 1996 to stop HIV from progressing into AIDS, to extend life expectancy and to reduce HIV-related deaths.
Under Montaner’s vision, B.C. became the “testing ground” for treatment as prevention — meaning that the treatment will help prevent the spread of the virus.
Starting in 1996, provincial health officials made B.C. the foundation for this treatment, testing the public and rolling out these drugs free of charge.
- Life in the forest: How Stanley Park’s longest resident survived a changing landscape
- Buzz kill? Gen Z less interested in coffee than older Canadians, survey shows
- Carbon rebate labelling in bank deposits fuelling confusion, minister says
- ‘They knew’: Victims of sexual abuse by Ontario youth leader sue Anglican Church
READ MORE: Doctors hope for cure in 2nd baby born with HIV
It worked: For every 100 patients using HAART, scientists recorded a three per cent decrease in HIV diagnoses in B.C.
New cases also took a steep decline — turns out, the cocktail also lowers the viral load of those who are HIV positive to the point where they are less likely to transmit the virus to their partners.
Canadian research backed up Montaner’s results: The National Institutes of Health suggests HAART decreases HIV transmission by 90 per cent.
In B.C., HIV diagnoses dipped from 18 per 100,000 in 1995 to 5.5 by 2012. Compare that to Saskatchewan where cases have multiplied from nearly three people per 100,000 in 1995 to 17 people 18 years later.
“No other jurisdiction in the country has seen anything that compares,” Montaner said.
The therapy’s been adopted in China, France, Brazil, Spain, Panama and Sierra Leone. Deals are in the works with Australia, Mexico and South Africa. The World Health Organization has even endorsed it.
But no other province in Canada covers 100 per cent of the HAART medication.
READ MORE: HIV/AIDS ward closes at St. Paul’s Hospital due to decline in disease
Montaner says he’s in talks with provincial health departments but Ottawa hasn’t responded to his requests to meet with federal health officials – or the Prime Minister.
“Every year, I get the same response. Thank you, but no thank you,” he said.
Correspondence provided to Global News by Montaner provides an example of his offer to walk federal officials through HAART’s success.
The Public Health Agency of Canada says it’s “closely monitoring” developments internationally but decisions on treatment and the delivery of health care services are a provincial issue.
(It also noted it spent $86.7 million on research, diagnosis and treatment in 2014-15 alone.)
The Prime Minister’s Office referred questions to Health Minister Rona Ambrose. Ambrose’s office said that since she was appointed, she’s met with “several organizations, announced a new research initiative towards finding a cure” and attended an AIDS gala.
“Our government takes the need to address HIV and AIDS very seriously and we will continue to work with our partners to find solutions,” the health ministry said in a statement.
In the meantime, some jurisdictions are going a step further: U.S. health officials are recommending hundreds of thousands of people considered at risk of contracting HIV/AIDS take a drug called Truvada to ward off the disease, even if they haven’t contracted it.
READ MORE: HIV isn’t easily transmitted by sex, Canadian doctors say
Prescriptions for Truvada are slated to increase to 500,000 per year from fewer than 10,000.
(Those considered at risk include anyone having sex with an HIV-infected partner; gay or bisexual men who have had sex without a condom or has been diagnosed with an STI; heterosexual men or women who don’t always use condoms with partners who may be at risk; and anyone who shares needles or injects drugs.)
The drug costs $13,000 a year and, according to U.S. reports, most insurers already cover it.
The CDC wouldn’t comment on Canada’s HAART therapy but it’s used in parts of the U.S., including San Francisco, New York and Washington, D.C.
Montaner hasn’t bought in: He’s concerned treating anyone at risk would mean the number of people who need to be treated could skyrocket.
“This is both an elusive number and an evolving number,” he said.
But he is still holding out for a national strategy in Canada.
“I remain hopeful that someday it’s going to happen.”
carmen.chai@globalnews.ca
Follow @Carmen_Chai




Comments