With a family doctor shortage, increasing burnout among health-care workers and ever-growing wait times at emergency departments putting more and more pressure on Ontario’s health-care system, the province’s doctors are hoping the government heeds their suggestions for solutions.

“We are in a state of dire consequence if we don’t do something, particularly around primary care,” says Dr. Andrew Park, president of the Ontario Medical Association.
Park is addressing the province’s standing committee on finance and economic affairs in Chatham, Ont., on Tuesday. On behalf of Ontario’s doctors, Park is pitching an 11-point plan to address weaknesses in the health-care system ahead of the province’s 2024 budget, with primary care the main priority.
“(Primary care) is kind of the backbone of our universal system; it’s the first point of access,” he explained.
“As an emergency physician, I’m seeing patients with more advanced disease. They’re presenting with, whether it’s cancers or other diseases that have been more advanced because they’ve been putting it off because they don’t have a family doctor. These things are more costly to the system. They’re more costly, most importantly, to the patient.”
Currently, there are 2.3 million Ontarians without a family doctor. By 2026, that number could reach 4.5 million, Park says.
He adds that part of the problem is simply unnecessary paperwork.
“Physicians are spending 19 hours a week on paperwork or administrative tasks. Now, some of those are going to be necessary, but some of them really aren’t. And we’ve seen an explosion of this number where doctors are spending more time in front of computers than they are in front of patients.”
Outside of family medicine, Park says another area of focus is addressing hospital overcrowding. He says roughly 10 to 20 per cent of patients at any given hospital do not need to be in an acute care hospital but do need some form of support.
“A fraction of those patients really could be at home if they had appropriate home care supports. Home care supports are less costly to the system overall and they support the patients at home where patients want to be and where, frankly, we can provide more effective care,” he said.
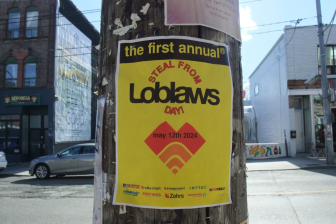
- Grocery code: How Ottawa has tried to get Loblaw, Walmart on board
- Alberta to overhaul municipal rules to include sweeping new powers, municipal political parties
- Norad looking to NATO to help detect threats over the Arctic, chief says
- Military judges don’t have divided loyalties, Canada’s top court rules
“But because we’ve had the inability to institute home care — whether it’s a physiotherapist or PSW (personal support worker) to help support those patients at home — they end up the only place it seems to be the catch-all for these patients, the security blanket, and that’s our hospitals.”
Hannah Jensen, spokesperson for the Ministry of Health, says the government understands that “the status quo isn’t working” and that plans are in place to address needs in primary care and home care and to reduce the administrative burden on physicians.
“We have invested $1 billion over three years into home care, accelerating investments as part of this year’s budget (23/24), introducing legislation to continue to modernize homecare; launched the largest medical school expansion in 15 years, including adding 44 new undergraduate and 63 new residency seats at the (Northern Ontario School of Medicine); expanded the Northern Ontario Resident Streamlined Training and Reimbursement (Nor-Star) program which removes barriers to training more physicians in Northern Ontario; broken down barriers for internationally and interprovincially educated healthcare workers to work in Ontario, including the new Practice Ready Ontario Program that will add 50 new physicians; and we are working with our healthcare partners to tackle the administrative burden on physicians.”
Jensen also says the province is actually leading Canada with 90 per cent of Ontarians having a primary care provider but acknowledged it is still an important issue.
“We are investing tens of millions of dollars to create new interdisciplinary primary care teams across the province. This is the largest expansion of primary care teams since they were established in Ontario. We received an overwhelming amount of applications in our Expression of Interest that closed in 2023. Details around successful applicants will be shared in the coming weeks.”
Meanwhile, Ontario is far from alone when it comes to pressures facing its health-care system. Last week, the Canadian Medical Association released a statement saying unless major systemic changes are made, the problem in emergency departments coast to coast will keep unfolding.
“I mean, the last 20 years, the emergency departments have become all things for everybody all the time because we’re always open, and the system is starting to reflect that crisis,” said Dr. Trevor Jain, an ER doctor with the Canadian Association of Emergency Physicians (CAEP).
“If you talk to any emergency department, we can stand being busy. We don’t mind being busy, but overcrowding kills and that’s what we’re starting to see.”
The OMA’s 11-point plan focuses on three priorities:
- Fix the crisis in primary care:
- Expand access to team-based care.
- Build a northern and rural physician workforce strategy.
- Reduce the burden of unnecessary administration:
- Create a centralized intake and referral system.
- Streamline forms and reduce sick notes and referral letters.
- Explore the use of artificial intelligence scribes.
- Improve Health Report Manager, an information-sharing tool between hospitals and family doctors.
- Increase community capacity and tackle hospital overcrowding:
- Appropriately fund home care and home-care providers.
- Expand programs that provide hospital-level care in patients’ homes.
- Embed care co-ordinators and home care within primary care and Ontario Health Teams.
- Provide long-term care homes with equipment to prevent unnecessary hospital transfers.
- Ensure all Ontarians have access to palliative care when they need it.
— with files from Global News’ Naomi Barghiel.



Comments