A Hamilton Health Sciences clinical pharmacist hopes there will be a day when naloxone kits will be as common across Canada as first aid kits, fire extinguishers and EpiPens, amid monthly opioid poisonings that are still fairly high nationwide.

Dr. Harsit Patel, an emergency medicine pharmacist at Hamilton General, says the medication is not just for those using illicit street drugs but also for people prescribed therapy who accidentally overdose.
“About 96 per cent of opioid overdoses are not intentional, they’re accidental,” Patel told Global News ahead of International Overdose Awareness Day on Wednesday.
“So my role as a pharmacist and hospital employee, when we get patients who overdose or just asking for a kit, is to educate them.”
Naloxone is not a complete treatment for suspected overdoses but a tool that gives a patient more time to seek critical help from professionals and ultimately a “positive outcome,” according to the pharmacy specialist.
“The thing with an opioid overdose, or someone not breathing and you suspect has an opioid overdose, is a response from paramedics that could take six to eight minutes,” said Patel.
“If the person is not breathing for six to eight minutes, the health outcome is not great.”
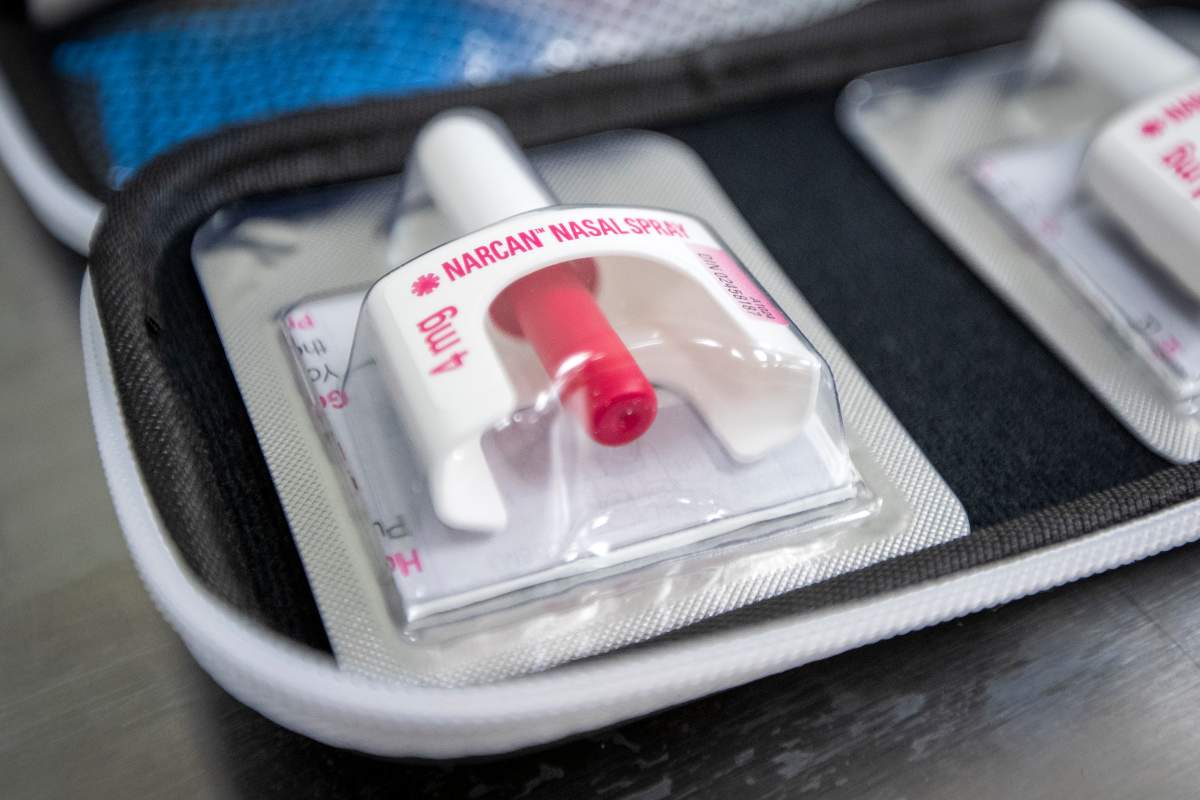
He says the medication comes in two forms, an injection or nasal spray, which essentially reverses the effects of an opioid and “kicks it off the brain,” allowing a person to breathe again.

Get daily National news
The nasal brand, Narcan, is the version that’s easier to administer, using a device with a little plunger that can be depressed to emit spray straight into the nose.
“The other kit is the intramuscular kit. This is the one that has a needle and is injected into a muscle within the body,” Patel said.
“I think a lot of people who may not be health-care professionals will find that cumbersome or hard to use.”
Patel says you only have to look as far as the most recent opioid numbers across Canada to make an argument for making the treatments more readily available to the general public.
Canada racked up 7,560 opioid-related deaths in 2021, with Ontario accounting for about 2,700 of those fatalities.
Hamilton had 166 probable or confirmed deaths related to opioids in the same time period.
So far in 2022, paramedics have responded to 489 suspected opioid overdoses in the city which shows some stabilizing month over month compared to cases last year.
“If we look at the numbers from the start of 2021 up until August of last year, there was about 594 that we had responded to,” said Hamilton Paramedics Supt. Dave Thompson.
“So it looks like the 2022 numbers are trending down, which is always a positive thing.”
In 2020 and 2021, city paramedics were responding to an average of two suspected opioid overdoses each day with the bulk of the incidents in the city’s core, particularly the downtown area.
The majority of cases (over 70 per cent) resides with the male population, with the average age of a victim around 36 years.
Thompson says the city’s most vulnerable, particularly those experiencing homelessness, are prime candidates for overdoses but says the affliction doesn’t discriminate as paramedics do respond to calls in a number of settings.
“We see them in residences, we see them out in public streets, it really varies,” said Thompson.
“An overdose can affect anybody, so really the goal and the aim is to increase awareness and encourage people to not only get trained in how to respond to an opioid overdose, but also administer naloxone.”
Last year the city hit a record number of suspected poisonings per month, averaging about 76 cases.
That number is down to about 66 as of the beginning of August.
Patel acknowledges the apparent year over year drop but says it’s still “significantly high” compared to pre-pandemic totals in 2019 which checked in at 50 per month.
Ontario made naloxone kits available to the general public through pharmacies without a prescription in 2016.
Since then Hamilton pharmacies have issued some 45,000 kits including about 15,000 in 2021.
In December, the city kicked off a collaboration with Hamilton paramedics using close to 400 trained paramedics to educate the general public on how to use the naloxone kits.
Nine months into the initiative, Hamilton Paramedics say they’ve trained and equipped 96 people.
Patel says those who may fear administering the treatment can take solace in the fact there’s no evidence of any negative health effects dispensing Narcan into a person not experiencing an overdose.
“But if you did give it when they are on opioids, you could potentially reverse their overdose and help them breathe again,” Patel said.












Comments