Executives with Hamilton’s hospitals served notice to the public on Thursday, revealing staffing shortages plaguing the system are creating service delays amid a seventh wave of COVID-19 that has arrived earlier than expected.

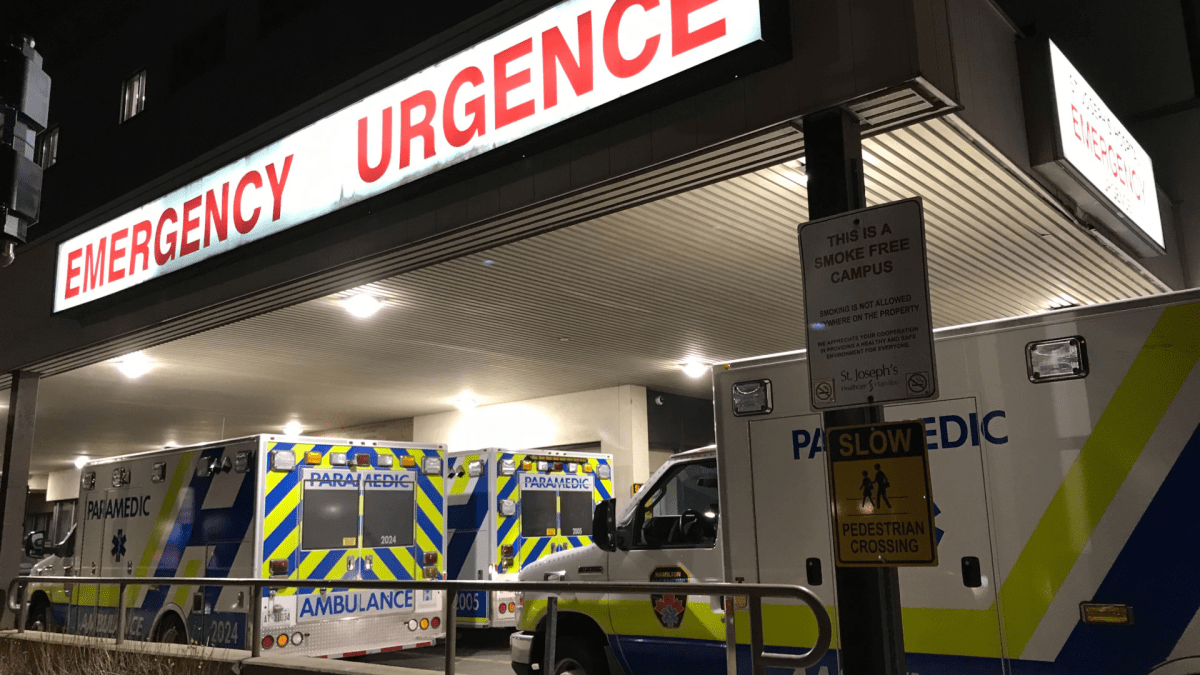
In a joint release, Hamilton Health Sciences (HHS) and St. Joseph’s Healthcare suggested the public should seek alternate healthcare options rather than a stop at hospital, if not an emergency.
“Despite aggressive recruitment efforts by both hospitals, the number of qualified applicants is often not enough to fill vacancies,” execs said in the statement.
“Staffing shortages are further exacerbated by a rise in the number of staff and physicians in self-isolation due to COVID, and a much higher number of staff off ill than usual.”
Combined, the networks estimate 350 staff and physicians are in self-isolation due to illness as of Monday.
Dr. Khalid Azzam, physician-in-chief at HHS, says the issue typically surrounds patients at high risk visiting a hospital for a procedure or treatment and being diagnosed with COVID after a pre-screening and test.
“This patient has to be isolated. They have to go through prevention of spread protocol,” Azzam told Global News.
“Then staff may become asymptomatic and not very sick, but still have to go off work and isolate for a significant period of time.”
During an HHS staff town hall last Thursday, executive vice-president and chief operating officer Sharon Pierson said the hospital was “not out of the woods” and that staff cannot let their guard down.
“Certainly health-care workers remain at high risk of exposure and would encourage everyone to get that second or that second booster just as soon as you’re all eligible,” Pierson told staff.

Get weekly health news
The networks say despite “aggressive recruitment” there are 675 job vacancies between the two hospitals as of Wednesday.
St. Joe’s chief emergency medicine and deputy chief of staff Dr. Greg Rutledge says increased patient volume, decreased HR resources, and upticks in staff illness due to the seventh wave are the factors currently hindering the system.
“We’re not seeing dramatic rises in our inpatients yet or in our ICU, but are seeing some of our staff having to go off sick with COVID again, which is further straining our resources,” Rutledge told Global News.
Both HHS and St. Joe’s estimate a combined backlog of 12,000 surgical cases with no projected timeline for resuming service at pre-pandemic levels due to the staffing issues.
Rutledge says the networks have been pursuing short-term and long-term alterations to the hiring process but expects service impacts will be an issue for at least several months if not much longer.
“We’re looking at alternate resources in terms of different skill sets that can provide supports on the floor in the emergency itself,” Rutledge said.
“So recognizing a significant vacancy, recognizing that our job fairs have not been as successful as they’ve been in the past, we have to start to look for other solutions.”
As of Thursday, HHS reported an overall staffing level of around 15,000 workers, including physicians. Around 5,700 were holding positions at St. Joe’s.
Azzam says expanding the networks pools nationally rather than just locally to bring in health-care professionals has helped to fill around 25 per cent of vacancies in the last few months.
Bringing on health-care aides to help registered nurses with some tasks — like serving meals, feeding patients and patient comfort — has also been one innovative solution.
However, he says they’ve not been able to do that in operating rooms which have strict provincial standards of care requiring staff with medical college certifications.
“We’re continuing with our traditional groups of health-care providers in the usual areas of emergency medicine, floor surgical floors and ICU,” said Azzam.
Both the HHS and St. Joe’s executives are suggesting residents not needing emergency care try a family doctor, an urgent care centre or Health Connect Ontario — where registered nurses are available by phone or web chat.
COVID transmission in Hamilton 'high and increasing,' according to public health
As of Wednesday, six of Hamilton Public Health’s key COVID-19 monitoring indicators showed increasing trends, including the seven-day average of new cases, which has moved from 62 reported on July 3 to 93 as of July 17.
Active institutional outbreaks have essentially doubled from 18 reported on July 5 to 31 as of Tuesday.
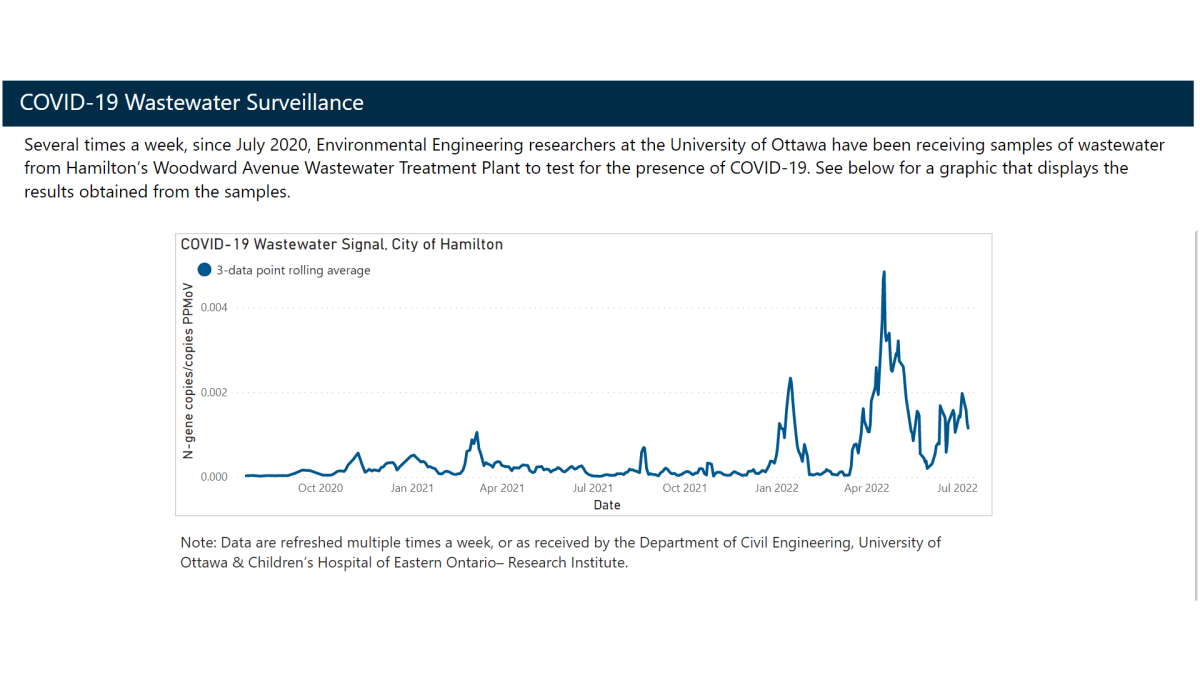
Wastewater viral signals detecting COVID-19 in samples have been steadily increasing since early June, closing in on levels seen in the initial Omicron wave in mid-January.
So far, an estimated 1.3 million doses of the COVID-19 vaccines have been administered in the city with 87.8 per cent of Hamiltonians aged five years and older having chosen to receive at least one shot.
Only about 55.6 per cent of Hamiltonians aged 12 years and older have received a third dose of a COVID-19 vaccine, as of July 21.
Around 37 per cent of those between the ages of 5 and 11 years old in Hamilton have received at least two doses of a vaccine.
A number of areas around the central Hamilton census tract continue to have the lowest second dose vaccination rates averaging around the 70-per cent mark as of Wednesday.














Comments
Want to discuss? Please read our Commenting Policy first.