It’s been more than four months since a Vernon woman with cystic fibrosis was forced to stop taking a life-changing medication because she can’t afford it.

Melissa Verleg said her health has declined significantly since she was forced to stop taking Orkambi.
“I have to be a spectator in my life again and there is no guarantee that I’m going to get any of that lung function back. I believe it is all because I came off Orkambi.”
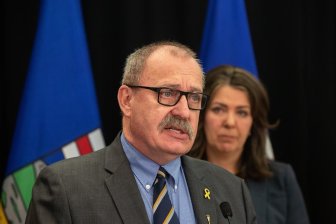
On Tuesday, Verleg and local Liberal MLA Eric Foster held a press conference to urge the drug company and the province to step up and provide Verleg with compassionate coverage for the pricey drug while wider issues of the drug’s coverage in British Columbia are worked out.
“Because of a power struggle between a major pharmaceutical company and the Minister of Health in the province of British Columbia, her health is deteriorating every day and they could fix it if they chose to,” Foster said.
- Alberta to overhaul municipal rules to include sweeping new powers, municipal political parties
- Norad looking to NATO to help detect threats over the Arctic, chief says
- Grocery code: How Ottawa has tried to get Loblaw, Walmart on board
- Military judges don’t have divided loyalties, Canada’s top court rules
Verleg has been on the drug for 18 months before she was forced to stop taking it because changes to her private insurance meant she no longer had the coverage to pay for the expensive drug.
She said the medication costs around $20,000 each month.
For months, Verleg has been lobbying the provincial government to cover the drug that’s changed her life.

The province previously declined to cover the expensive medication after a review said, “There is insufficient evidence to conclude that this drug will improve cystic fibrosis outcomes.”
Vertex Pharmaceuticals, the company behind Orkambi, called the Canadian authorities’ assessments of the drug surprising and untrue.
Now the rules for those national drug-coverage reviews have changed and Vertex Pharmaceuticals has re-submitted Orkambi for review by the Common Drug Review.
However, even if the review recommends Orkambi be covered, it could be a long wait before patients like Verleg have funding for the drug.
“It could be as much as a year before it gets through all the other processes,” Foster said.
The provincial health ministry said that it needs to wait for the drug-review process to take place and that any compassionate coverage would be up to the drug company.
“British Columbia is committed to an evidence-based process that includes at its centre the Common Drug Review’s determinations of a drug’s clinical efficacy and cost effectiveness,” the Ministry of Health said in a statement.
However, Foster contends the province does have the power to provide coverage for Verleg.
He pointed to the example of a $750,000-per-year drug called Soliris which, last year, the provincial health minister said would be covered on a case-by-case basis.
The province said there are different circumstances for different drugs and it has done as much as it can on the Orkambi file by advocating for another review of the drug through the national Common Drug Review process.
“In the case of Soliris, five other provinces use Soliris to treat aHUS on an exceptional basis, and we were able to take advantage of their collective experience when making the decision last year to provide it on exceptional case by case basis.”
Vertex Pharmaceuticals said it won’t discuss individual cases for privacy reasons.
However, the business has not offered compassionate coverage to Verleg.
– with files from Estefania Duran and Emily Lazatin



Comments