EDMONTON – As concern grows over the mounting number of deadly fentanyl overdoses in Alberta, the province has taken action to make the drug’s antidote – Naloxone – more accessible.

But an Edmonton doctor says that while the government’s Naloxone policy is a good thing, another effective treatment should also be used – methadone.
READ MORE: Health minister pleased fentanyl antidote naloxone will soon be prescription-free
Dr. Hakique Virani says the methadone clinic at the Metro City Medical Clinic, where he serves as medical director, has never been busier.
“We’re seeing people from the suburbs of Edmonton – St. Albert, Sherwood Park – who are young, just finishing high school, have promising futures ahead of them (but) who have gotten caught up in this opiate problem,” he said.
Virani says methadone or Suboxone are medications that prevent opioid withdrawal and reduce cravings for addicts.
“We have patients who have been on treatment for eight or nine years who may stay on it for decades or longer, who have productive jobs and good family lives and relationships.”
According to Virani, methadone treatment is the most effective way to treat opioid addiction but the problem is there’s a wait list to receive treatment at every clinic.
READ MORE: Rising fentanyl abuse spurs need for public education: Alberta group
- ‘Super lice’ are becoming more resistant to chemical shampoos. What to use instead
- Solar eclipse eye damage: More than 160 cases reported in Ontario, Quebec
- Invasive strep: ‘Don’t wait’ to seek care, N.S. woman warns on long road to recovery
- Canadian man dies during Texas Ironman event. His widow wants answers as to why
Since February, the Notley government has added one new methadone program while adding over 40 new detox beds.
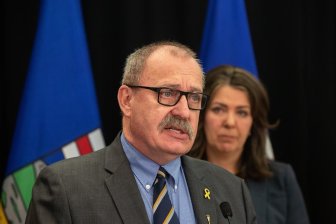
“We are adding detox beds to help people who want access to treatment because we have seen that there’s a need out there in the community for it,” Associate Minister of Health Brandy Payne said.
Virani says the government is too focused on promoting abstinence through expensive detox programs.
“The scary thing is, is those (beds) may do more harm than good,” he said.
Global News spoke to a mother of an opioid addict who also believes more emphasis needs to be placed on methadone treatment. Petra Schulz’s son Danny had been on methadone for several months but once he ended the treatment, he relapsed and died a year later after taking a fentanyl pill.
“The night before (Danny died), he had actually asked me to make an appointment again with his counsellor, which I had done, but he never was able to go to that appointment,’ Schulz said.
According to Virani, the relapse rate for opioid users after detox is 90 per cent.
Stopping opioid use lowers an addicted person’s tolerance, which puts them at a higher risk of overdose and death and Schulz said she believes her son would still be alive if he had stayed on a methadone treatment.
“We have this idea that drugs are bad,” Schulz said. “And indeed they are, but it’s unrealistic to think that we will keep all people off drugs.”
Currently, there are nine methadone clinics across the province.
With files from Su-Ling Goh.



Comments