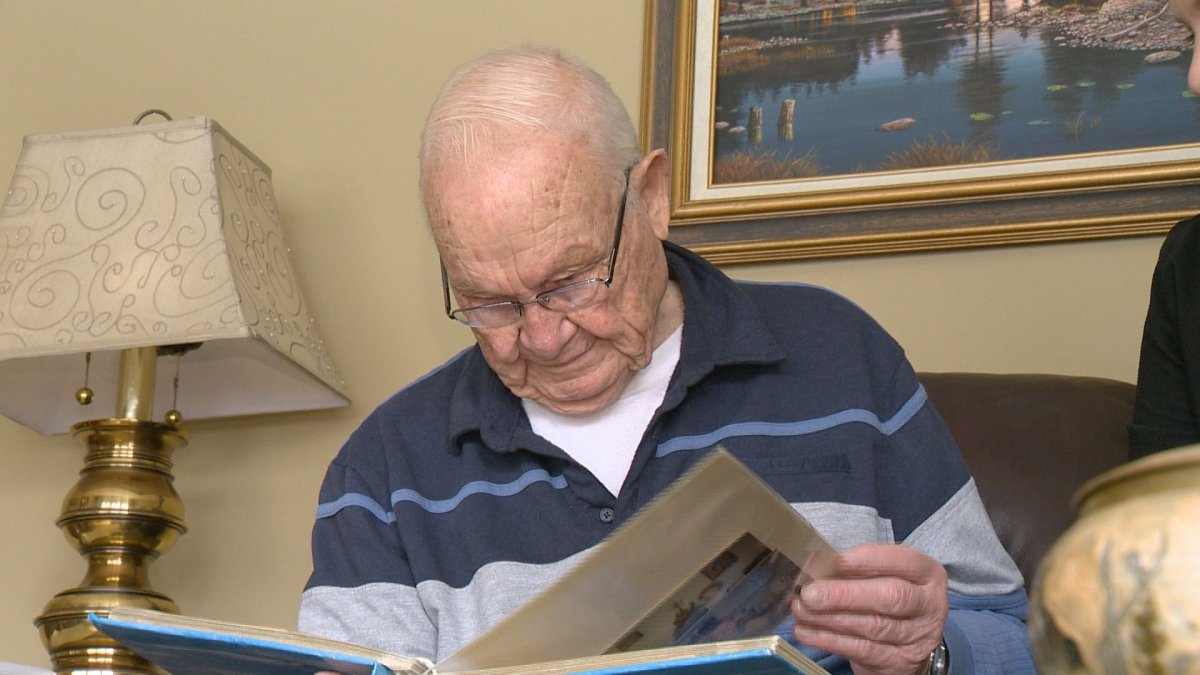
Jim Brass and his wife Marion spent a wonderful 59 years together, but their last 31 hours were a real struggle.

Marion had previously been diagnosed with chronic obstructive pulmonary disease. She was in palliative care in late July, but was discharged after she started feeling better.
Two weeks later, Jim took her into emergency because her health took a turn for the worse. That’s where she would spend the last 31 hours of her life.
“It was like a revolving door. Mom was right by the exit, and so it was also where they were cleaning the bedpans. It was incredibly busy and noisy and people walking in and out,” Marion’s daughter Dana said. “It was extremely disruptive, not calm and peaceful.”
“I think in the last hours of your life it would sure be nice to go out in dignity and peace,” Dana said.
“I think this is sort of a symptom that when there’s not enough beds and there’s not enough nurses, they’re run off their feet like this, that’s where our biggest issue is. That in the final 30 hours of mom’s life, it was a pretty miserable way to go out and not very humane.”
“It wasn’t a very good place to die, it was just a thin curtain pulled around,” Jim said.
The family was desperate for Marion to be sent to a proper hospital bed or transferred back to palliative care, but they were told the hospital was short six beds.
- Canadian man dies during Texas Ironman event. His widow wants answers as to why
- ‘Shock and disbelief’ after Manitoba school trustee’s Indigenous comments
- Canadian food banks are on the brink: ‘This is not a sustainable situation’
- Invasive strep: ‘Don’t wait’ to seek care, N.S. woman warns on long road to recovery
“I broke down crying while I talked to those nurses. I mean literally begging, is there any way, can you put her in the hallway up here, just anything,” Dana said. “I was just beside myself.”
The average wait for a hospital bed after being admitted to emergency is 24 hours and for palliative care is 14 hours.
“The health region can’t speak to specific cases, but patients are prioritized based on need, and it is a concern when they don’t get the service they need,” Sheila Anderson, Regina Qu’Appelle Health Region’s Urban Services Executive Director, said.
“I think it’s fair to say it’s hard for any of your loved ones to die, anywhere, anytime. I think the emergency room is a very busy place and I think our staff do a really good job in there to try to be thoughtful and compassionate, but I think that it’s a busy environment,” Anderson said. “We have really limited space for people to have private areas, so I would say it’s not ideal and not what we would hope for.”
“Patients and families have an opportunity to call our client advocate office, and those often are the best times that we get our learning, when we’re face to face with clients and hearing about the improvements we could make,” Anderson said.
The Brass family is hoping by telling the story of Marion’s final hours, other families won’t need to go through the same pain.
“My mom looked out for everyone. She looked out for the little guy. She liked to speak up when there was an injustice,” Dana said. “She wouldn’t want another family to go through what she went through, or what we’ve gone through.”
“I think in the last hours of your life it would sure be nice to go out in dignity and peace.”



Comments