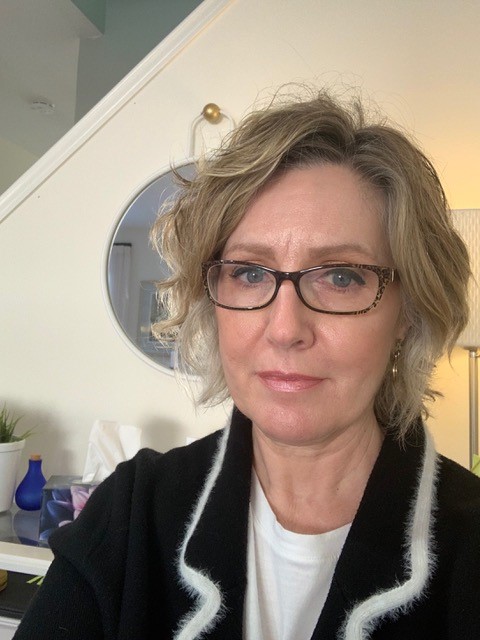
For 63-year-old Maureen Meehan, being proactive and mindful of the harmful effects of the Sun has always been a priority. So, when the London, Ont., resident received a stage 3 melanoma diagnosis back in 2017, it came as a major shock.

“It started as a small mole on my right forearm,” she explained. “But when I noticed it had changed, so did my mindset and I went to pursue this and get it checked out.”
The mole on her forearm had been there for many years, but Meehan said that once it started “feeling funny and itchy,” it was time to see her family doctor. She said that she was initially dismissed before the spot proved to be cancerous.
“I went to see a specialist who did a punch biopsy where they take a sample of the optimal tissue and sent it off to the lab. He said that I might not hear from him in a couple weeks, so when I got a call about two days later, I was shocked to hear that I had malignant melanoma,” she said.
Meehan said that the fatal form of skin cancer had metastasized quickly and spread to her lymph nodes.
“My first thought was for my family,” she recalled. “When you first hear that you have cancer, it’s frightening. … Skin cancer can be invasive, and it can be one of the deadliest forms of cancer.”
Luckily, Meehan said that her diagnosis was caught early. She had surgery on her forearm to remove the melanoma as well as two lymph nodes from her right armpit.
Now officially one year into remission, she’s sharing her story to spread awareness about the importance of early detection, encouraging others to be vigilant about new or existing moles.
“Have your skin checked regularly, and sometimes you need someone to check places that you can’t see,” she said. “Heading into the summer, this is something to take seriously and not dismiss at all.”

According to the Canadian Cancer Society, roughly 9,000 people were diagnosed with melanoma in 2022 and 1,200 people died from it.
The foundation also states that women with melanoma skin cancer tend to have a better prognosis than men.

Get weekly health news
“This may be because women more commonly develop melanomas that involve the extremities, while men more commonly develop melanomas that involve the trunk, head or neck,” the Canadian Cancer Society states on its website.
Additionally, while people younger than 35 have a greater risk of the cancer spreading to nearby lymph nodes, the foundation said that those older have a “poorer prognosis.”
But according to onco-dermatologist Dr. Maxwell Sauder, melanoma is something that “we don’t talk about enough.”
He said that melanoma is a cancer of the skin’s pigment-producing cells in the skin, and it normally tends to present itself as irregular-looking moles.
“It certainly is one of the deadliest forms of skin cancer there is,” he said. “But if caught early, it’s extremely easy to manage and take care of which is why creating public awareness for skin surveillance is crucial.”
The majority of melanoma cases can be found anywhere on the body, more commonly on sun-exposed areas, including the back and calves, the Toronto-based doctor explained.
“When melanomas are caught early, meaning that they’re limited just to the skin, the cure rate is the highest out of almost any cancer that there is,” Sauder said.
“Where people get into trouble is when melanoma progresses beyond the skin. It has the ability to unfortunately spread to lymph nodes — that’s generally where it goes first — and then it can spread to distant organs such as the lungs, liver, brain, bones, etc. That’s when it can be deadly.”
However, he added that over the last 10 to 15 years, there’s been an “explosion” of effective treatments for melanoma, highlighting the strides made in the treatment of Stage 3 and Stage 4 melanoma.

Sauder recommends that people pay close attention to the size, shape and colour of moles, referring to the “ABCDE’s” of melanoma:
- Asymmetry – If you were to cut the mole in half, would it be different on either side?
- Border – Is the border of the mole irregular in any way? Are there any jagged edges or finger-like projections?
- Colour – Is the colour of the mole not the same throughout? It could have shades of three or more different colours.
- Diameter – Is the mole larger than a pencil eraser (approximately six millimetres)?
- Evolution – Have there been any dramatic changes?
“That is the most important point,” said Sauder, referring to evolution. “Anything changing dramatically in a three-to-six-month period, whether it’s size, shape, colour, even things like itching, burning, pain, or bleeding on a regular basis — that’s something that people should get examined by a healthcare practitioner.”
He also stressed the importance of loved ones and family members, saying they “play an important role in early detection.”
“About 53 per cent of melanomas are discovered by the patients themselves. But in addition to that, a further 17 per cent are actually detected by family members,” he said. “It’s about being completely aware of your body and taking a quick inventory of your moles once every one to three months could potentially help you identify something that’s changed over that time period which could ultimately save someone’s life.”
Sauder also recommends using “safe sun practices,” such as wearing SPF-graded sunscreen, avoiding tanning beds and minimizing time spent outside in periods of ultra-high ultraviolet rays.
Going back to Meehan, she stressed that melanoma skin cancer can happen to anyone.
“If I hadn’t been as proactive, if I hadn’t been mindful about checking my moles, then we wouldn’t be having this conversation today,” she said.













Comments
Want to discuss? Please read our Commenting Policy first.