TORONTO — When a mental health crisis call comes in to 911 in certain parts of Toronto next month, a team typically consisting of two people such as a harm-reduction worker and a nurse, or an Indigenous elder and a de-escalation expert — not police — will be the first to respond.

The mobile unit will meet with the individual in crisis and figure out what they need. Response teams will then check on the person within two days and help arrange further support, such as long-term counselling, as required.
It’s all part of a new approach to crisis intervention in Toronto that’s beginning with a pilot program launching in a few weeks.
The City of Toronto — which plans to eventually implement the program in all neighbourhoods — describes the effort as a community-led, trauma-informed alternative to traditional crisis response, with a focus on reducing harm and preventing problems from arising.
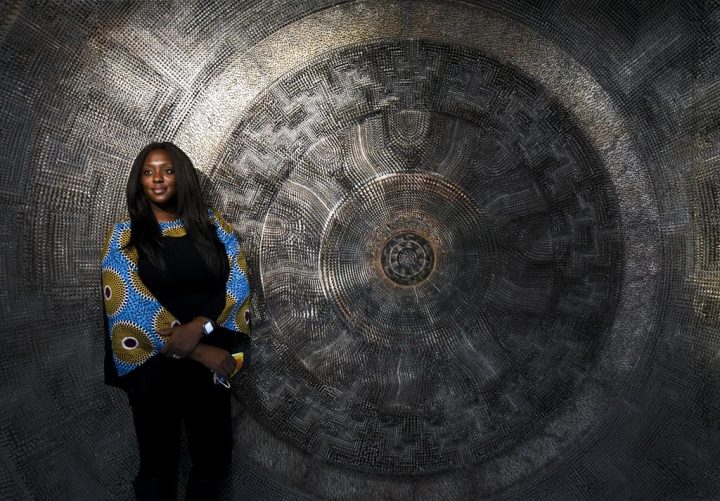
“The idea is that we don’t need a law enforcement approach when the issue is a mental health crisis, a substance abuse crisis, that those are health issues, they’re not criminal issues,” said Denise Andrea Campbell, the city’s executive director of social development, finance and administration, who is leading the program.
“The appropriate response (is) health supports, not enforcement officers.”
The pilot program will operate in four areas of Toronto where apprehensions under the Mental Health Act and 911 calls for people in crisis are the highest.
At first, calls to 911 will be funnelled to the new community crisis support program, but eventually, Campbell said, mental health crisis calls can go straight to 211 — Ontario’s community and social services helpline.
The new program is the product of community consultations and research into similar models in 50 jurisdictions around the world, Campbell said. Through that research and community feedback, the city decided to go with a non-police crisis response model, she said.
A team will only call for police support if its members are not able to de-escalate a situation and a crisis call turns violent. But Campbell said evidence from similar models has shown that is hardly ever the case.
“For example, in New York, their B-HEARD teams, in their first six months, they responded to 564 calls and only six per cent of those calls required the assistance of the (police),” she said.

Get daily National news
Initially, the pilot program will launch in northeast and downtown east parts of the city next month. In June, two more pilots will launch in a northwest and downtown west area.
The city said the pilots will allow it to test, evaluate and revise a non-police-led crisis response before implementing the program on a larger scale. Citywide implementation is expected by 2025 at the latest, Campbell said.
Toronto police Staff Supt. Randy Carter said the force is “very excited” for the new service.
“They’re a more informed service because it’s done through crisis workers who have lived experience of special training, more extensive training than our police officers at de-escalating people that are in crisis,” he said.
Carter noted that Toronto police respond to roughly 32,000 crisis calls a year where there’s no criminality or violence involved. In some cases, he said there’s an “anxiety that exists and builds” when officers respond to those calls.
The new service will allow police resources to be used for other matters, Carter said.
“There’s many other things to do, both in a proactive and reactive way … to make sure that people are feeling safe,” he said.
The TAIBU Community Health Centre, which delivers programs and services for Black communities across the Greater Toronto Area, will be responsible for leading the northeast pilot of the new program.

Executive director Liben Gebremikael said the centre is in the process of hiring for the program, noting that the region’s mobile crisis team will be made up of individuals with lived experience around mental health and addiction issues, anti-Black racism, Indigenous-specific racism or other kinds of discrimination.
Those team members will be able to “connect to people in a better way” given their lived experience and will work to build trust with community members to provide early interventions, Gebremikael said.
“Our ultimate kind of ideal goal is that people are able to seek and find support before they get to a crisis. If people have gotten to a crisis situation, that’s already too late,” he said.
“Obviously, we’re going to still have some crisis response. When we get there, our aim is that our service will be a culturally and community … appropriate response that would take people’s lived experiences and other social determinants of health into consideration and provide a warm and wrapped-around response.”
Dr. Andrew Pinto, a family physician at St. Michael’s Hospital in Toronto, said a community-led approach to helping people in mental health crises is “long overdue” and has the potential to save lives.

Pinto said it could lead to more support for those who live with mental health concerns and could prevent cases where they are harming themselves or others. In the long term, he said it can help people engage with health and social care and other resources.
Since police won’t be going to confront someone who’s in a mental health crisis, the risk of “police committing violence and actually killing somebody” could also be reduced, he said.
“I think that this type of approach can make a difference for folks. And I think that a really rigorous evaluation will help confirm (that),” Pinto said.
TAIBU’s Gebremikael agreed, saying the new service is “a long time coming.”
“This is really now time for change,” he said.
“The painful experience of incidents like the (murder of) George Floyd … has brought this a little bit faster … but at least we are here today, the city has really stepped up, and this is the time to really test this.”






Comments