Many of Canada’s seniors ingest a worrying, and perhaps unnecessary, amount of medication, according to the lead author of a new study that found a Canadian-made electronic tool is effective in safely reducing the medication overload.

The study by the Research Institute of the McGill University Health Centre (MUHC) was conducted with patients 65 and over who took five or more medications a day. It found doctors could safely reduce the number of medications given to their patients by using MedSafer, an electronic tool that helps monitor the different medications and flag potentially inappropriate ones.
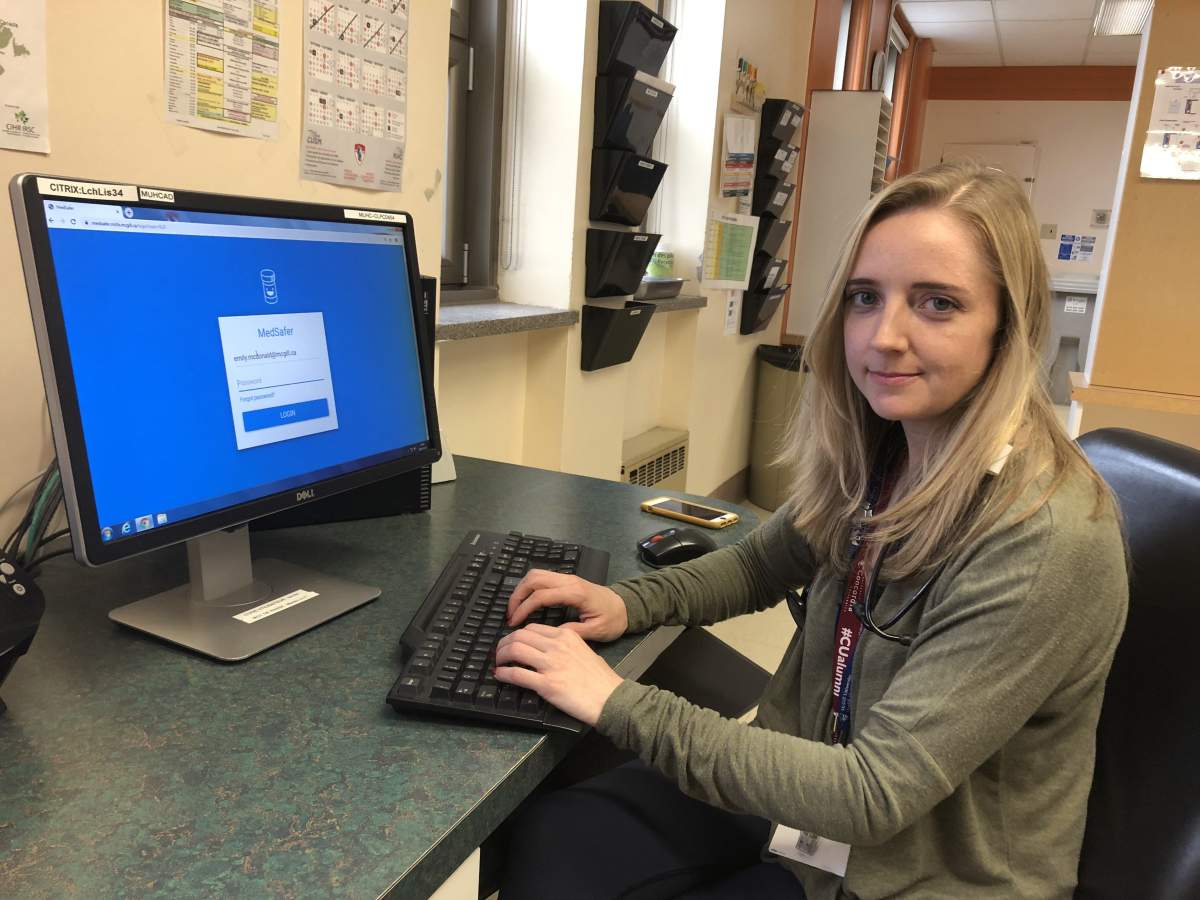
Lead author Emily McDonald, a researcher and internal medicine physician at the McGill University Health Centre in Montreal, said taking multiple medications can be dangerous to people 65 and up, who are vulnerable to side effects.
READ MORE: Seniors being over-medicated a growing concern, says doctor
Currently, some 40 per cent of older adults take five or more medications per day. In addition to the risk of side effects or complications, McDonald says some medications may not be appropriate for certain health problems, which can make seniors vulnerable to additional hospitalizations, memory problems, dizziness, and balance problems that lead to falls and fractures.
“It’s one of the most common causes of hospital visits,” she said in a phone interview.
“In seniors, polypharmacy — taking multiple medications — has increased enormously in recent years. We’re talking about taking five, 10, even 15 medications.”

Get weekly health news
While lists of potentially harmful medication combinations exist already, it can be complicated and time-consuming for doctors to research them, especially when several people are involved in a patient’s care.
READ MORE: Why some doctors want people to take less medication
“Performing a prescription checkup is a complex process for interprofessional teams, and often involves complicated decision-making,” she explained.
A desire to address the problem led McDonald and study co-author Todd Lee to create MedSafer. It checks the different combinations of medications prescribed to a patient and offers a recommendation of whether any can be safely stopped or reduced. Designed specifically for seniors, the tool can be used by doctors, pharmacists and nurse practitioners.
The goal of the study, published in September in the Journal of the American Geriatrics Society, was to see if the tool was useful in tapering off medications, and if it was safe to do so.
“Often, clinicians don’t want to stop a medication because they’re afraid of causing secondary reactions for the patient in withdrawing the medication,” McDonald said.
The study took place between Sept 2016 and May 2017 with 1,066 hospital patients at four research centres in Montreal, Ottawa and Toronto.
An initial report by MedSafer showed that 82 per cent of the subjects were receiving a potentially inappropriate medication. That triggered a review by a doctor, who made the final decision on whether the medication was necessary.
Later, the researchers compared the results of patients whose doctors had used MedSafer to those who had received the usual care. It found that 54.7 per cent of patients in the MedSafer group had had a medication de-prescribed by the time they were discharged, compared with 46.9 per cent for the second group.

The researchers believe the difference may be even greater in other clinical settings where there are fewer drug experts on site, such as long-term care homes.
Following the results of the study, MedSafer will be deployed in long-term care units in New Brunswick and Ontario. In Quebec, McDonald is hoping to start a pilot project at Lachine Hospital, part of the McGill University Health Centre.
McDonald said the researchers interviewed the patients and their families a month after leaving hospital and found the health of the MedSafer group was no worse as a result of the reduction in medication.
“There was no increase in no adverse effects,” McDonald said. “It’s safe.”
READ MORE: Health care is a top election issue, but many don’t want to pay more for it: Ipsos poll






Comments
Want to discuss? Please read our Commenting Policy first.