

By
Skye Bryden-Blom &
Rebecca Lau
Global News
Published April 5, 2024
4 min read

This is the latest instalment in a Global News series called Code Critical, which examines the issues impacting the health-care system in Nova Scotia. The full series can be found here.
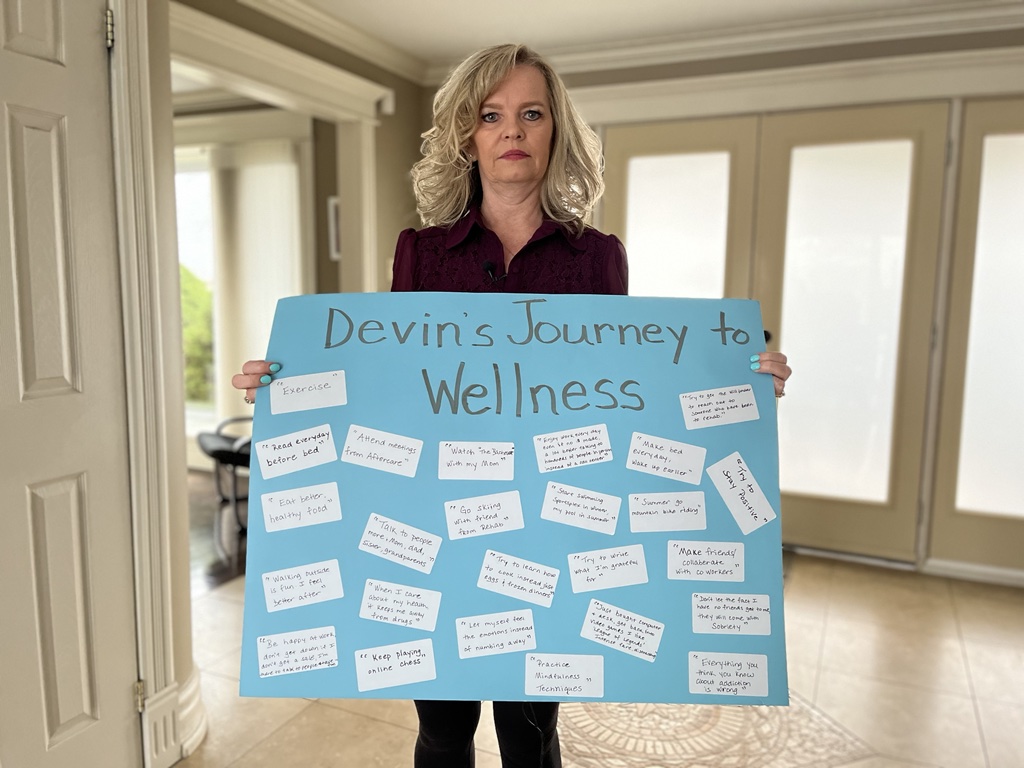
For Christine Kidd, the memory of her son is what gives her the drive to fight for change.
Devin, 26, died from a drug overdose a month ago after a long and difficult battle with addiction.
Over the years, Kidd has stood by her son’s side while navigating a system of rehab, detox, psychiatrists, walk-in clinics and emergency services.
Ultimately, she believes the health-care system failed him.
“He kept saying, ‘I want to get sober. My dream is to have a home and a family,'” Kidd recalls.
“He doesn’t have a voice now, so I have to be that voice and I want something done. Something has to change.”
Kidd describes Devin as a smart and funny young man with a big heart. He excelled at sports and played nine years of hockey with the Dartmouth Whalers.
But his struggles, she says, began in high school when he started experimenting with marijuana.
“I was reading through his notes from rehab. They made him write a letter to his 18-year-old self. It was heartbreaking to read that, but it said in there he got some weed in high school and someone told him, ‘Congratulations, you just spent $10 on a feeling,'” she says inside her Darmouth home.
As time went on, she says he started using pills, including Xanax, and other benzodiazepines — a class of depressants.
Things escalated from there and his mental health began to decline.
“It was always something he was trying to use to mask things, to numb his feelings, you know?” she says.
“He always made me laugh. He was just funny, fun to be around, just a bit of a goofball…. Gradually we started seeing a different person and we were very confused, like, ‘What’s going on?'”
She says Devin wanted to get help, so the family tried everything from counselling to spending $15,000 on a private 30-day rehab program.
They also tried to get him admitted to hospital when a walk-in clinic doctor wrote a referral that called for immediate support due to his suicide risk.
“Just back in February, he had called the crisis line. It was five times in a matter of two weeks. We had the ambulance and police here,” she says.
“He went to the Dartmouth General and they took him to the QEII to talk to psychiatry. Every time, they just sent him home the next day.”
Later that month, he did get into a detox program at the hospital for five days.
“He was sober, he was himself. It was a breath of fresh air,” she recalls.
But the relief was short-lived. Kidd says there was no followup and on March 17, her son died from an overdose.
“I really think it was an accidental overdose. He had a lot of plans. He was making plans to get back to work, which he loved.”
Kidd says she’s sharing her family’s story because she wants to see the health-care system reach a point where it has a better capacity for addictions-related hospital stays. She also believes followup care is vital when a patient is released.
In a statement, Nova Scotia Health spokesperson Brendan Elliott says the department offers their sympathies to Devin’s family and friends.
While the department can’t comment on individual cases for privacy reasons, he says the decision on whether to keep someone in hospital is “made by gaining an understanding of the whole person – not by a single moment or incident.”
“Nova Scotia Health’s Mental Health and Addictions program operates on a provincial bed system. If someone is assessed as requiring a bed, they will not be turned away,” he writes.
“It’s important to stress a mental health and /or addictions crisis does not necessarily require hospital-based assessment or interventions.”
He goes on to say that “discharge planning” for a person begins when they are admitted and is done by a multidisciplinary team.
“A discharged patient is always given follow up options depending on their need with appropriate services,” he writes.
But Kidd doesn’t feel that was their experience.
Instead, she says her son felt abandoned.
“I think it was last year. He said, ‘I’ve called, I’ve tried this, I’ve tried that.’ And he goes, ‘Nobody cares. They don’t care,'” she says.
That’s why Kidd wants addictions to be viewed differently: like any other illness in our health-care system.
“If someone has cancer, has an illness, they’re getting the help. They’re getting the appointments to follow up, they’re getting all that,” she explains.
“And drug addiction can enter any family. It doesn’t discriminate. It doesn’t matter.”
Anyone experiencing a mental health crisis is encouraged to use the following resources:

Comments
Want to discuss? Please read our Commenting Policy first.