The abortion pill Mifegymiso comes to Canada this spring but it may not make abortions accessible to Canadians who can’t access them now – at least not at first.

Health Canada approved the drug, a combination of mifepristone and misoprostol previously known as RU-486, last year.
Unlike most drugs available in Canada, Mifegymiso will only be prescribed by people who are registered and trained in its use; methadone is regulated similarly.
READ MORE: How the abortion pill could change reproductive health
Online training modules organized by the Society of Obstetricians and Gynecologists of Canada will start later this month, the society says. (They wouldn’t give more details; nor would distributor Celopharma or the national College of Family Physicians.)
But some abortion providers worry initial restrictions on who’s allowed to prescribe the drug and what procedures are required beforehand won’t make it any more accessible than surgical abortions are right now.
READ MORE: Where in Canada can you get an abortion? It’s secret
When the drug first becomes available, only physicians will be able to prescribe and dispense it, even though the U.S. Food and Drug administration now allows anyone with prescribing authority, which in at least 13 states includes nurse practitioners and midwives, to administer it.
And Health Canada’s monograph says women need to have ultrasounds before they can get the drug — even though women who live far away from abortion providers may also live far away from ultrasound clinics.
“It’s going to roll out in a very restricted way,”says Suzanne Newman, a Winnipeg-based doctor who provides abortions.
“I have no idea how soon we’ll be able to provide these in remote locations.”
READ MORE: Abortion access still depends on who you are and where you live
Vicki Saporta, president of the National Abortion Federation in the U.S. and Canada, says there’s no reason to make ultrasounds a requirement.
“There’s no evidence to support that an ultrasound is necessary to provide safe and effective medical abortion care. So it’s unfortunate that they’re making it a requirement, and may impede some women’s access to the care.”
You also don’t need special training or registration to be able to administer the abortion pill in the U.S., Saporta said.
“It shouldn’t be required in Canada, either,” she said.
“I don’t think it’s going to be that onerous, but it should not be necessary for the safe and effective administration of the combination of mifepristone and misoprostol.”
READ MORE: How the abortion pill works
For many people, a major selling point of the abortion pill is its relative ease of access compared to surgical abortion which, while a relatively simple surgery, means travelling to a place that provides them.
“This is what’s ideal: to use this medication in remote areas to save these women trips,” Newman said.
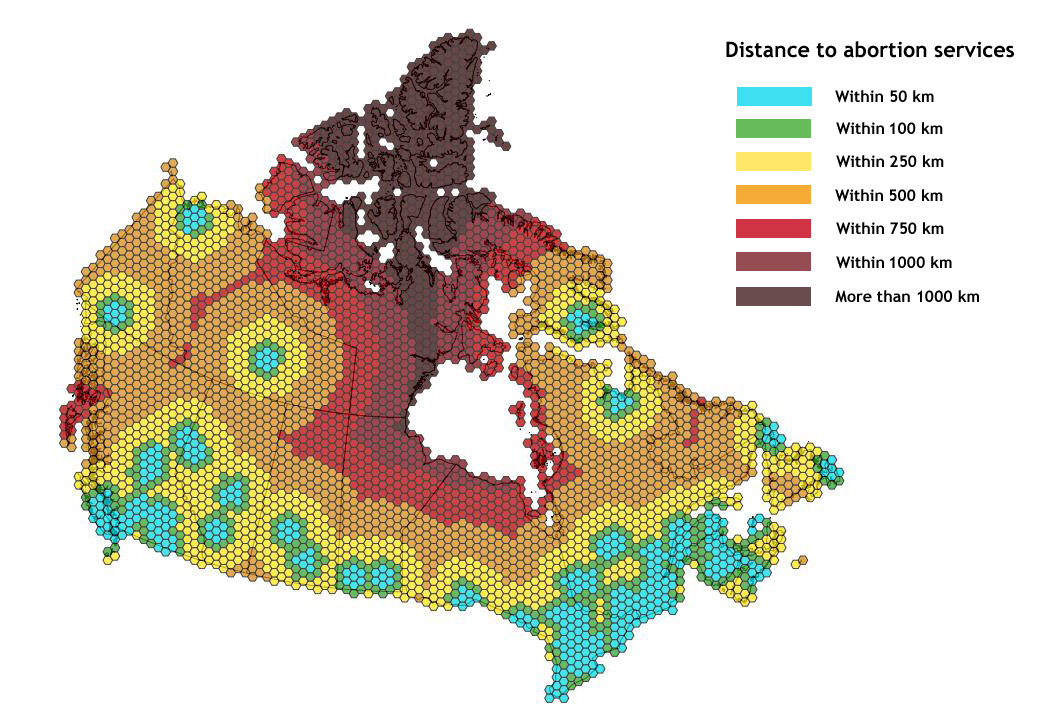
As Global News has reported, women living in much of the country face significant barriers getting reproductive care — higher barriers than other health services, given the judgment involved with telling a clinician, colleague, doctor or relative you need an abortion.
Newman has seen firsthand the geographic limits on abortion access: A 14-year-old, pregnant after being raped, whose doctor in rural Manitoba wouldn’t refer her because she was “too young” for an abortion; a young mom from Thompson who had to pay for the flight, hotel and abortion out of her own pocket because her health card was out of date.
The abortion pill has been used in other jurisdictions for decades. And in countries where it’s been around for a while, there tend to be fewer restrictions on its use.
This week the U.S. FDA loosened restrictions on the abortion pill south of the border: American women can now take it up to 70 days into a pregnancy, compared to 49 days as outlined by Health Canada.
A U.S. study published last month suggested telemedicine could make abortion more accessible to women living far from clinics: A trained physician can talk to the patient and oversee the administration of the drug from a distance.
Availability of the abortion pill means women who need to terminate pregnancies terminate them earlier, Saporta said.
In Canadian communities that don’t have a doctor full time, some have suggested, a nurse practitioner could administer the drug under the electronic supervision of a doctor. The U.S. now allows anyone with prescribing authority to administer the abortion pill.
READ MORE: PEI will start offering abortions
An ultrasound is the gold standard in determining how far along a pregnancy is and whether there are complications. But it isn’t the only way, Newman said.
“Many practitioners in Europe and even the U.S. are not using ultrasounds” before administering the abortion pill, she said.
Other unanswered questions include whether provinces will cover the cost.
“We’re hoping they cover it, and we’re working to promote that,” Newman said.
“If they don’t cover it, it kind of backfires because then it’ll be only women who can afford it.”
The provinces are waiting on the result of a Common Drug Review by the Canadian Agency for Drugs and Technologies in Health‘s Drug Expert Committee. The committee will make a recommendation as to whether provinces should pay for the drug, and then the provinces and territories will discuss whether to pool resources to buy the drug.
READ MORE: How abortion access varies across Canada
In the meantime, health practitioners are trying to prepare for Mifegymiso’s rollout.
“We’re trying to get ready, so it’s kind of difficult, definitely. … There’s still not a lot of information out there,” said Patricia LaRue, director of Gatineau’s Clinique des Femmes,
“We want to make sure that it’s safe for everyone, but we also want to make sure that its accessible, that it increases access to abortion. … I’m sure there are ways to make it safe and accessible at the same time.”
Federal Health Minister Jane Philpott wouldn’t comment on the rules governing Mifegymiso’s use, but said access is an issue for everyone in remote areas, regardless of the health service they need, and she’s trying to fix that.
“We look forward to working with our partners from all the provinces and territories to make sure that medically necessary care is accessible to Canadians regardless of where they’re from, regardless of their ability to pay for it.
“That’s my mandate.”



Comments