An Ontario doctor says taking ‘Socks Off’ in a primary care setting could be a step in the right direction in reducing a rising number of lower limb amputations across the province connected with diabetes and vascular disease.

Hamilton Health Sciences (HHS) together with the Greater Hamilton Health Network (GHHN) is launching the campaign, called Socks Off, on July 17, with goals to reduce the number of lower Hamilton, Ont., residents who lose a foot to amputation due to diabetes and/or vascular disease.
Dr. Brian McKenna, a family doctor and deputy lead physician at Hamilton Health Sciences, is hoping the late July campaign will push more health-care providers to add foot checks to routine diabetic visits in hopes of combating Ontario’s high amputation rates.
“In short, we want clinicians to tell patients to get their socks off in the office during routine diabetes visits so that we can inspect feet to prevent downstream outcomes related to wounds, ulceration and amputation,” McKenna explained.
Cuts, blisters, cracks and callouses are just some of the signs of poor circulation and potentially unhealthy blood vessels that contribute to the problem, according to McKenna.

Get weekly health news
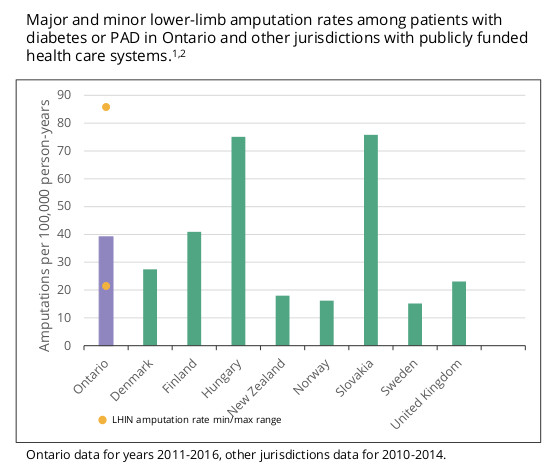
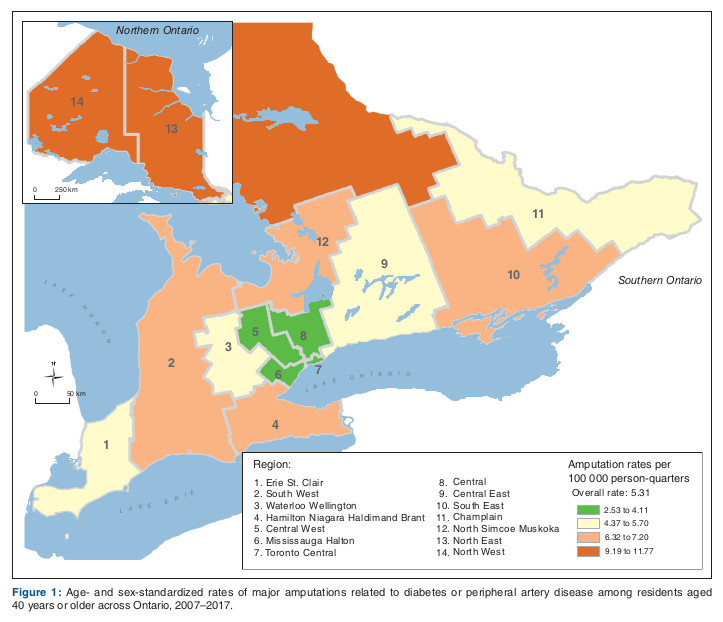
Hamilton finds itself in one of the Local Health Integrated Networks with a high rate of amputations connected with heart disease and diabetes.
Cases are most prominent in Hamilton’s lower end primarily due to sociological issues connected with poverty and health equity.
Diabetes is the leading cause of nontraumatic lower limb amputation in adults living in Canada and is associated with about 70 per cent of amputations performed in hospitals.
Foot ulcerations will affect 15-25 per cent of people living with diabetes over their lifetime.
Adults living with diabetes are 20 times more likely to undergo non-traumatic lower limb amputations, with 85 per cent preceded by foot ulcers.
Laura Hoffe, senior manager of policy for Diabetes Canada, wants federal and provincial governments to step up initiatives to mitigate amputations through affordable and timely access to medications, devices, education, and care necessary to achieve optimal diabetes management.
- What is Nipah virus? What to know about the disease as India faces outbreak
- Head-Smashed-In Buffalo Jump heritage site enjoys boost after shout out on ‘The Pitt’
- Pizza Pops contaminated with E. coli tied to 7 hospitalizations, data shows
- Pizza Pops E. coli recall grows as roughly a dozen products now hit
“People who experience a lower-limb amputation undergo tremendous emotional and financial distress,” Hoffe said.
“We also urge people with diabetes to check their feet daily for cuts, cracks, bruises, blisters, sores, infection and unusual markings.”
Ontario’s health care system is expected to take a $1.7 billion hit due to diabetes with about 80 per cent of that attributed to treating complications in acute care settings.
Improving blood sugar control through medicines and diet as well as kicking bad habits like smoking can prevent the progression of the peripheral vascular disease for those already with diabetes, according to McKenna.
“I do really think this demonstration is going to provide some good data that can help to underpin the kinds of long-term solutions that we need to change these numbers,” he said.











Comments