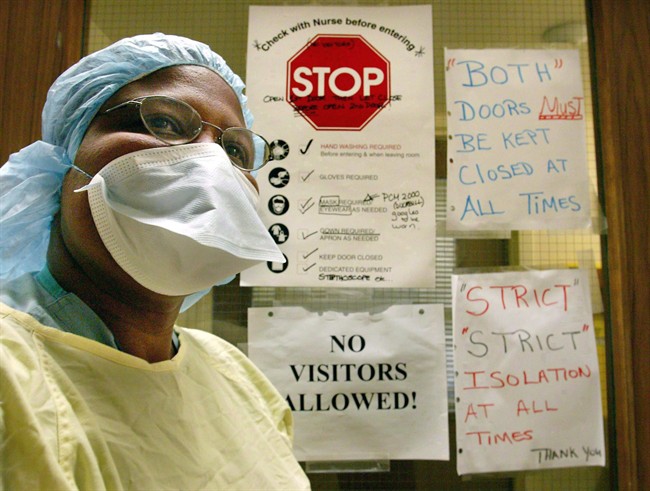
TORONTO – For the people who fought Toronto’s devastating SARS outbreak in 2003, the news out of South Korea right now sounds eerily familiar.

A man infected with a new coronavirus for which there are no vaccines or drugs turns up in a hospital sick and infectious. It is days before he’s recognized as a carrier of the new disease and during that time he isn’t isolated.
He infects a couple dozen people who, in turn, pass the disease to still more. The widening circle involves hospital patients, family members who visited them and health-care professionals who cared for them.
Cases start popping up in other hospitals. The public gets spooked. Authorities order exposed people into quarantine as they struggle to get ahead of a fast moving outbreak.
That could almost be a recitation of the early days of Toronto’s SARS outbreak. But South Korea is battling a cousin virus, Middle East respiratory syndrome or MERS.
READ MORE: 9 things you should know about MERS
Right now there is a lot of sympathy for the South Koreans among people who work in Toronto’s hospital and public health sectors.
“All of us who went through SARS — you know what they’re going through. It’s very similar and you understand what they feel like,” says Dr. Allison McGeer, head of infection control at Mount Sinai Hospital and a SARS survivor.
“They will get through it. But it’s just such an awful thing to happen to people.”
- Canadian man dies during Texas Ironman event. His widow wants answers as to why
- ‘Sciatica was gone’: hospital performs robot-assisted spinal surgery in Canadian first
- Canadians more likely to eat food past best-before date. What are the risks?
- Treatment from female doctors leads to lower death rates, study finds
As of today, South Korea is reporting 87 cases and six deaths. In the past 24 hours alone, the case count jumped by 23.
Dr. Bonnie Henry is British Columbia’s deputy provincial health officer. But in March 2003, when SARS hit, she was an associate medical officer of health for the City of Toronto.
Henry admits she gets “this feeling in my stomach” when she hears dispatches from the MERS front in South Korea.
READ MORE: SARS 10 years later: Doctors monitoring new coronavirus
She’s not alone. Dr. Brian Schwartz, Public Health Ontario’s chair for communicable diseases, emergency preparedness and response, says for many health-care professionals who fought SARS, the MERS news evokes a “visceral” response.
An emergency room physician, Schwartz was vice-chair of the SARS scientific advisory committee back in the day. He says the South Korean outbreak isn’t making him nervous. But he is driven to do all he can to ensure Ontario’s health-care system remains vigilant, so that if a MERS case shows up at a hospital in the province, the disease isn’t given the chance to take off.
With SARS, Toronto’s outbreak was already well underway when authorities realized a critically ill man suspected of having tuberculosis was actually dying of a new disease that would touch off big outbreaks in China, Hong Kong, Taiwan, Vietnam and Singapore.
Early on Henry and McGeer went to the first hospital in the Toronto chain, Scarborough Grace, to try to determine how many people had been exposed and might be infected.
“When we looked back on it and pieced it together there were 15 cases by the time we recognized that this person probably had this disease that was happening in China. Some of them were in hospital and some of them were in the community. Some of them were health-care providers,” Henry says.
All those ill people were exposing multiple others to the disease. Sick health-care workers started booking off work.
READ MORE: French doctors say incubation for MERS virus may be 12 days, recommend longer quarantines
“And we realized they were in multiple parts of the facility. They were nurses, they were X-ray techs…. The security guard in the emergency department. So it became very clear within a short period of time that there were people that we didn’t know who had been in contact (with the first case),” Henry says.
“And then there were health-care workers who were sick who’d been in contact with other health-care workers. And it sort of snowballed. And we had to make the decision to close the hospital.”
That cascading effect seems to be happening in South Korea. In Toronto, transfer of patients among hospitals brought the virus to more facilities. There are currently at least six hospitals that have been involved in the South Korean MERS saga.
Both outbreaks had a patient or patients who infected many others early in the outbreak. In Toronto, one of the earliest people to catch SARS infected 36 other people in two hospitals.
Though there are many similarities, there are differences too. When SARS hit Toronto, it didn’t yet have a name. MERS hit the world’s radar in September 2012 and has made headlines off and on ever since, mainly for cases on the Arabian Peninsula.
There was no test for SARS for much of the global outbreak, which burned out within four months. There is now a test for MERS. But a test only assists if you think to use it.
READ MORE: 2 new disease – H7N9 and coronavirus – could both spark global outbreaks
“It’s a way of saying ‘Yes’ or ‘No.’ But it doesn’t help if you haven’t recognized that the person has a respiratory infection to start with. And that’s where we need to focus, is on catching people early,” Henry says.
There is another difference: When SARS arose, no one knew what it was or whether its spread could be contained. That successful fight — as well as more than two years of experience containing MERS outbreaks in the Middle East — gives the South Koreans critical knowledge on what it takes to stop MERS.
That experience may also give the broader public health community some confidence MERS can be controlled. But it may not be making the South Koreans more reassured at the moment, McGeer admits.
“The fact that somebody else tells you it’s going to be over does not necessarily make you feel any better when you’re in the middle of it.”


Comments