The patient who died in the Edmundston Regional Hospital emergency room waiting area in December 2022 had been dropped off by their care home without anyone with them, according to documents obtained by Global News.

The details are the result of a New Brunswick Right to Information and Protection of Privacy Act (RTIPPA) claim filed by Global News – after being initially denied the records – which revealed the timeline and circumstances surrounding the death.
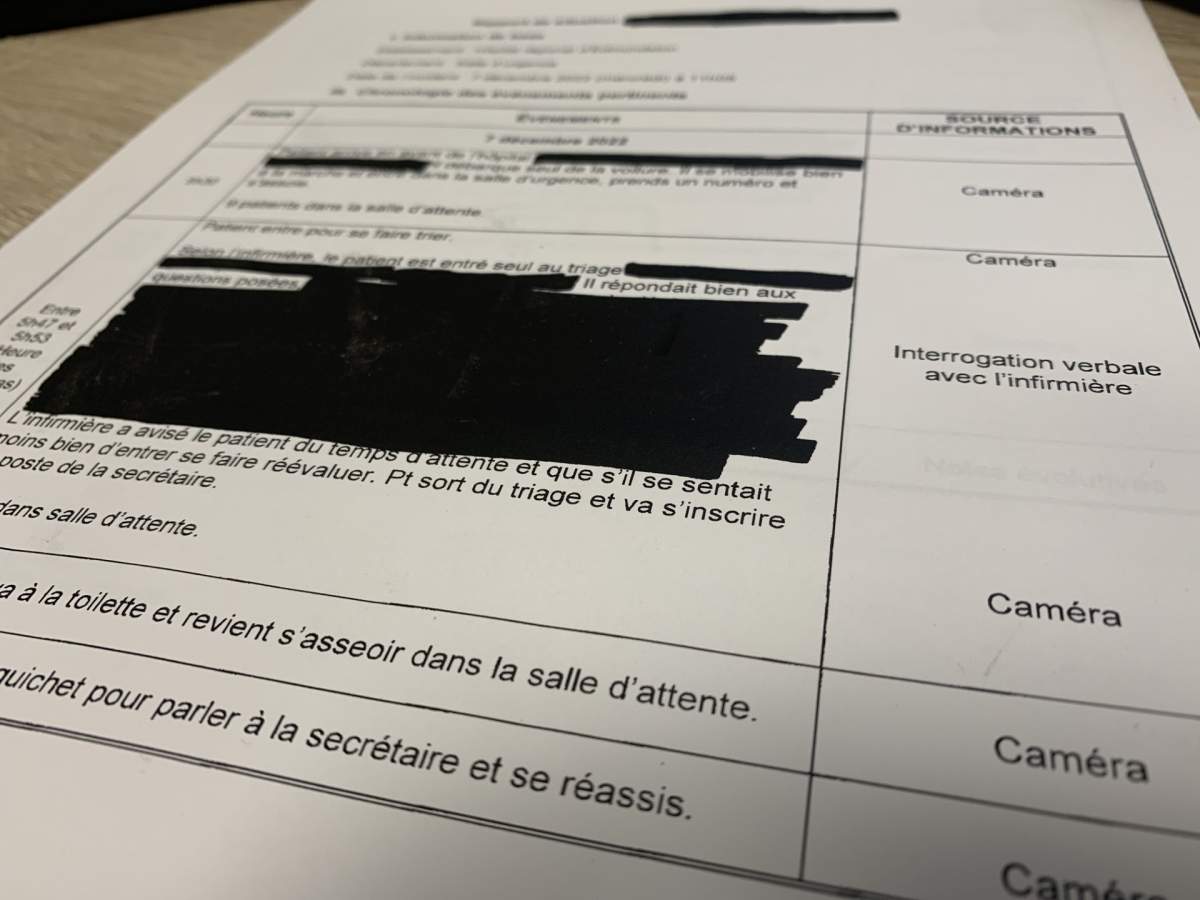
The timeline
The patient, who was reportedly 70 years old, arrived at the Edmundston Regional Hospital at 5:30 a.m. on Dec. 7, 2022.
Documents translated from French to English say he was mobile and answered questions well upon triage. Documents say he entered triage alone. Follow-up emails and documents, show the patient was a resident of a care home, unaccompanied on their trip to the ER.
“The nurse informed the patient of the waiting time and that if he felt less well, to come in, he would be reassessed,” the documents read, translated from French.
The patient was triaged at Level 4 – in accordance with the Canadian Triage Acuity Scale – which means less urgent care but should be seen within an hour of arrival.
Documents showed the ER wait times for a level 4 triage was up to 24 hours. Hospitals in the province have been grappling with staffing shortages for years, coming to a head in recent months.
Two other patients have died in New Brunswick emergency room waiting areas in the last year.
The timeline of information was gathered from the CCTV camera in the ER waiting room in which the patient is seen waiting. He goes to the bathroom a couple of times and attempts to get a drink from the vending machine.
At 10:43 a.m., the patient is seen going to the bathroom again.
Approximately 22 minutes later, the patient “leans a little forward in his chair, he makes a motion with his finger towards the COVID person and his head leans calmly … against the wall, very pale.”
Hospital staff are alerted by the woman screening people for COVID at the entrance and ER staff begin cardiac massage.
More than five hours after arrival, the patient was pronounced dead at 11:26 a.m.
Review the standards
The death has prompted advocates to call for a review of a social development policy and standards that, in some cases, allows patients and residents of adult residential facilities to be dropped off at an emergency department without someone staying with them.
The Department of Social Development confirmed, “in some cases, a staff from the home may drive a resident to the hospital if this is feasible, however, staff are not able to stay at the emergency room with the resident because they have to remain at the home.”

All public care homes are operated under the Adult Residential Facilities Standards, and they do not have medical advisors, whereas nursing homes in the province do.
Under those standards, “the ARF operator must ensure that the relevant information accompanies the resident sent to the hospital. This includes their Medicare number, medications they are taking, information on allergies and conditions”

Get weekly health news
“The standards also note that, when it is possible, the operator ensures the resident is accompanied by another individual,” the department said in an email.
It also said the next of kin or family member must be notified.
But it remains unclear why this resident was left alone.
Jan Seely, with the New Brunswick Association of Special Care Homes, said bringing about a specific rule to require people to stay with residents could be difficult given every situation is unique.
She said there are nearly 7,000 New Brunswickers living in care homes for many different reasons.
“The best scenario is that families would be able to spend that time with their loved one, as they are in a vulnerable situation, but when that can’t happen I know operators do their very best to get someone in there,” she said in an interview.
When a resident doesn’t have family or a next of kin nearby, Seely said it can make the situation more complicated.

Nursing homes do have access to on-site medical advisors, but agree with the assessment the situation would need to be individualized.
“In nursing homes, we really focus on a person-centered approach … so everyone needs to be looked at as an individual and focusing on their strengths and compensating for their losses,” said Julie Weir, CEO of the New Brunswick Nursing Home Association. “This means that some might be able to stay by themselves, but there needs to be support and a plan in place.”
Within the documents, it shows coroner Joe Kavanaugh was consulted on the case, and specifically went out of his way to say residents should be accompanied, “because sometimes they cannot properly express/examine their pain.”
Seniors advocate Cecile Cassista said she was distressed to hear the resident had so clearly fallen through the cracks.
“Well one of the questions I was questioning: the person living in a home, now it wasn’t clear whether it was a memory care home or whether it was level one or level two, but they’re in that home for a particular reason because they are not able to do things on their own,” she said in an interview.
She wants the standards to be reviewed, saying it seems like this individual was let down by both the health-care system and social development.
“The policy needs to be strengthened to ensure that when someone in these care facilities is taken to the hospital someone is with them at all times,” she said.

The Canadian Union of Public Employees represents thousands of employees in care homes and nursing homes in the province.
Jason St-Onge, 1st vice president for the council of nursing home unions, said it is feasible staffing shortages could prevent staff from staying with residents.
Many homes have different ways of implementing standards, he explained, making knowing what each would do in a specific case difficult.
He said in some cases, nursing and care home staff are a resident’s family. He said the sector is in crisis, trying not to become emotional when speaking to Global News.
“Residents can’t have a bath, they have to eat their meal cold because we don’t have (enough) hands, we don’t have the bodies on the floor to take care of them 100 per cent,” he said in an interview. “At the end of the day, a lot (of the staff) leave the work in tears, sad, mad, because they can’t offer 100 per cent of what those vulnerable people need.”
The patient at the ERH allegedly only had $2.60 in his pocket, as noted by the coroner. It’s unclear whether the patient was able to purchase food, having been seen going to the vending machine at least once on camera.
The recommendations
Vitalite Health Network said it has reviewed all the recommendations made by the Harmful Incident Review Committee – which were never made public.
There were five:
- Follow up after social development to ensure that the process for transferring a patient from the nursing/care home to the emergency department is followed to ensure patient safety.
- Develop and implement actions, in the short term, to be able to free up hospital beds quickly in order to unclog the emergency room
- Ensure that the HRE overflow plan is reviewed, implemented and adhered to in order to improve patient flow and ensure proper bed management
- Create a patient care attendant position in the emergency department waiting room to check the vital signs and well-being of patients waiting to see a doctor
- Evaluate the possibility of implementing the use of a device for the vital signs of patients, in the waiting room, targeted by the nurse at the triage
In an email, the health authority said it has completed recommendations two and three.
The email said the first recommendation, dealing with the safe transfer of patients, was also completed, adding discussions with social development had taken place. It did not elaborate on what those discussions were or whether there would be any changes to the standards as a result of the death.
Recommendation four, which is already implemented at Horizon Health Network in its major ERs following a waiting room death in June, has not been completed – with the health authority saying it hopes to have it done by December 2023, a year after the death.
The final recommendation was rejected by the RHA, saying a study did not provide conclusive results.
The Adult Residential Facilities Standards was last revised in September 2013, but the Department of Social Development said it regularly reviews policies and standards to ensure compliance.








Comments
Want to discuss? Please read our Commenting Policy first.