As Ontario’s Progressive Conservative government halts the opening of three new overdose-prevention sites to review if they “have merit,” experts say the decision could have dire consequences amid an opioid crisis that is killing Canadians in record numbers.

Health Minister Christine Elliot said that sites set to open in Thunder Bay, Ont., St. Catharines, Ont., and Toronto will be put on hold as the government examines “evidence on both sides” of the debate on the facilities’ role in saving lives and getting people into drug treatment programs.
READ MORE: Ontario safe injection, overdose prevention sites in limbo
“There is evidence on both sides,” Elliot said during question period Monday. “We need to make sure that we review all of the evidence to understand what is happening. What is happening that is saving lives? What else can we do to save more lives? Are there other examples that we should be looking at besides supervised injection clinics?”
Experts and advocates on the frontlines of the opioid epidemic, however, say there is already an overwhelming body of evidence to show that the overdose-prevention and safe injection sites save lives and help get people into treatment.
“Halting the construction of new sites will unquestionably lead to more deaths,” said Dr. David Juurlink, the head of clinical pharmacology and toxicology at the University of Toronto. “The crisis that we are now in requires multiple different interventions to prevent people from dying by the thousands. These are one of those interventions.”
“It’s very clear they reduce deaths.”
READ MORE: Are opioid deaths reducing our average life expectancy? Canada now investigating
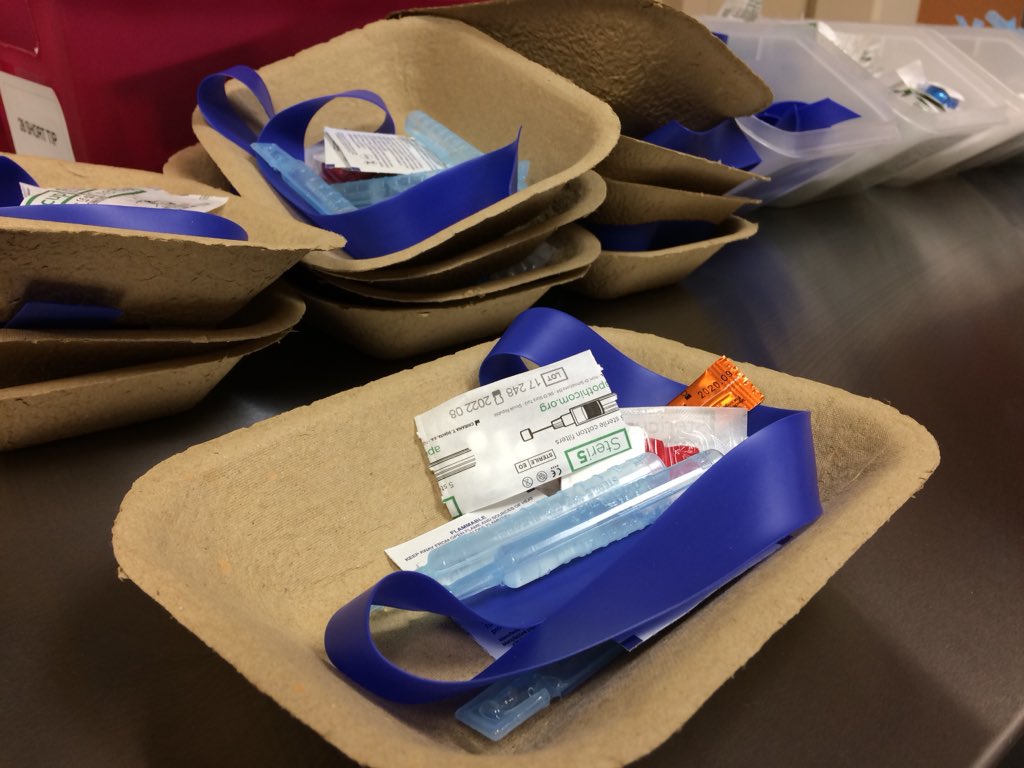
Overdose-prevention sites are temporary facilities approved by the province to address an immediate need in a community by providing monitoring for people at risk of an overdose, reducing harm by supplying items such as clean needles, and by facilitating referrals to mental health and substance treatment services.
Supervised consumption sites — also known as safe injection sites — require federal approval. These are permanent facilities that provide safe environments where people can use substances under the supervision of trained staff, offer clean injection supplies and help connect people to health care services, including treatment.
What does the research say?
Studies on these facilities conducted in Canada and around the world have shown they are not only life saving but connect people with long-term addiction treatment, reduce the spread of HIV and hepatitis C, and ultimately save healthcare dollars.
One study published in 2011 examined overdose mortality in the two years before and after a supervised injection site opened in Vancouver in 2003 known as InSite. It found the fatal overdose rate in the area decreased by 35 per cent.

Get weekly health news
Other studies conducted on InSite found it prevents anywhere from six to 57 HIV infections per year and decreases the average length of hospital stays. And while these facilities have been accused of fostering drug trafficking, a review of studies have found no increase with respect to drug trafficking or assaults/robbery in the areas. One study actually found a decline in vehicle break-ins and vehicle theft.
“The evidence for the effectiveness of these sites is not only compelling, it comes from a period of time when the illicit drug supply was not littered with fentanyl,” Juurlink said. “The risk of dying from an overdose is greater than it’s ever been. These sites, as a result, are even more important.”
WATCH: Nearly 4,000 Canadians died of opioid overdoses in 2017, a new record
A study from 2010 in Sydney, Australia, found a supervised injection facility led to fewer ambulance calls for treating overdoses.
In 2017, researchers at the Lankenau Institute for Medical Research in Pennsylvania developed models to measure how many drug overdose deaths could be prevented and how much money could be saved with a supervised consumption facility in Philadelphia. They found that up to 76 drug overdose deaths annually could be prevented and that, in terms of skin and soft tissue infections alone, the city would save as much as US$1.8 million in hospitalization annually.
In Europe, some countries have used safe injection sites for decades. Switzerland created its first drug consumption room in 1986.
The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) — using three decades of research — concluded in 2017 that supervised drug consumption facilities led to “safer use for clients” and “wider health and public order benefits.” The review also found many benefits similar to Canada, like the reductions in drug-related deaths, a decrease in emergency calls related to overdoses, and greater referrals for drug addiction treatment.
“These sites have been shown to improve overall community safety by moving drug use inside as opposed to alleyways and parks, and they build relationships so they make referrals health care services and addiction treatment,” said Nick Boyce, with the Toronto Overdose Prevention Society.
The cost of delays
Boyce said with the more 1,200 overdose deaths in Ontario in 2017, the decision to delay opening new facilities will put people at risk.
“Thunder Bay has the highest rates of opioid deaths in the province,” he said. “In Parkdale, a neighbourhood in Toronto, workers there say they are losing people on a monthly, if not weekly, basis.”
In Hamilton, 87 people died from opioid overdoses last year. Shelter Health Network is operating the city’s only temporary supervised injection site in collaboration with Hamilton Urban Core Community Health Centre.
WATCH: What you need to know about opioid overdoses in Canada

Executive director of the centre, Denise Brooks, said she is eager to share the success of her facility with the Ford government.
“We’ve noticed that there is a reduction in the amount of overdoses,” Brooks said. “And people are starting to be more open, or asking even, ‘What are the programs I can go to for support?’”
“The proof is out there already, so you wonder what else is being looked at?” she said. “The concern is what happens to people in the meantime.”
Asked what evidence Ontario’s Ministry of Health might be reviewing to suggest these facilities are not successful, a spokesperson for Elliot said the minister was “emphasizing that she is undertaking an evidence-based review.”
“Listening to experts from various backgrounds, to ensure that any continuation of Supervised Consumption Services and Overdose Prevention sites are going to introduce people into rehabilitation and ensure people struggling with addiction get the help they need,” Hayley Chazan said. “That’s why the ministry has indicated that no new sites should open to the public at this time.”
WATCH: Ottawa introduces regulations to protect safe injection sites

The review is expected to be completed by the end of September.
Premier Doug Ford had previously said he is “dead against” supervised injection sites and believed the focus should be on drug rehabilitation instead.
“If your son, daughter, loved one ever had an addiction, would you want them to go in a little area and do more drugs? I am dead against that,” Ford said during the election. “We have to help these people. We can’t just keep feeding them and feeding them.”
But Juurlink takes with critics who say tax payer dollars and resources are being wasted on people who are using drugs.
“People who use these sites will very often seek out addiction care and try to stop using,” he said. “But they have to do that at their own pace.”
“If someone dies six months or a year before they decide that they really want to get their lives in order you don’t have that chance,” he said. ”You can’t rehabilitate someone who is dead.”



%20AUG%2015%20STILL00000000.jpg?w=1200&quality=70&strip=all)














Comments