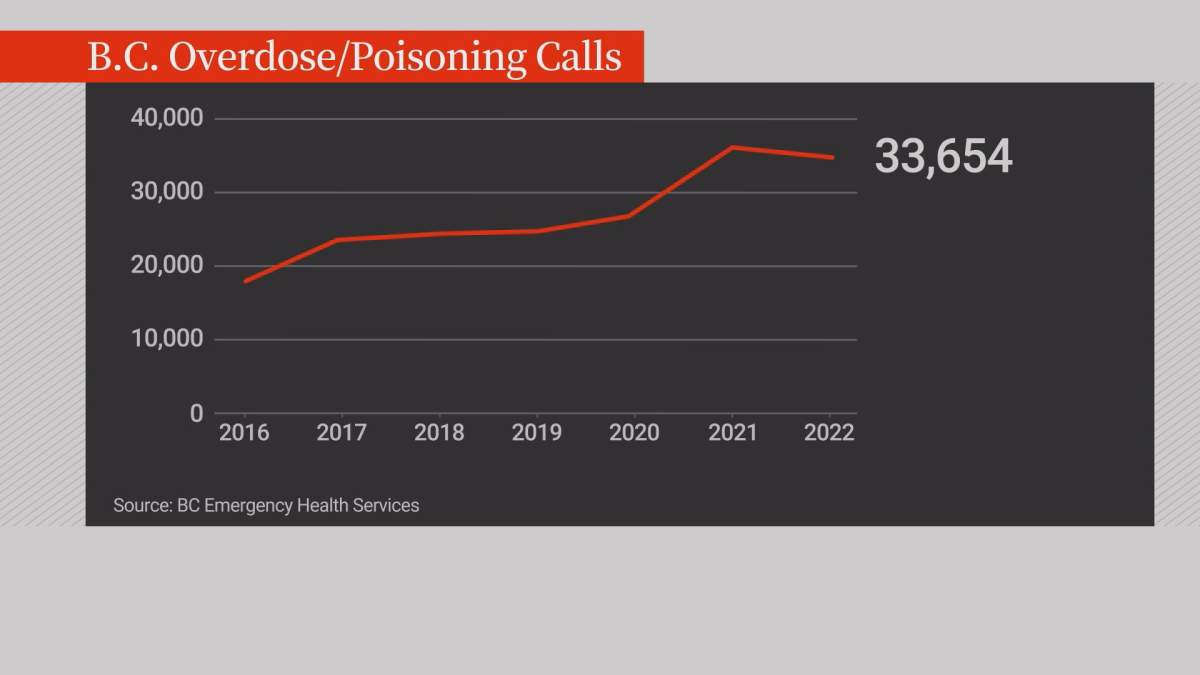
BC Emergency Health Services (BCEHS) has released its annual stats on the number of overdose and poisoning calls paramedics were dispatched to.

The numbers show that throughout B.C., the call volumes were down last year, but that decrease was led by the Vancouver Coastal Health and Fraser Health regions.
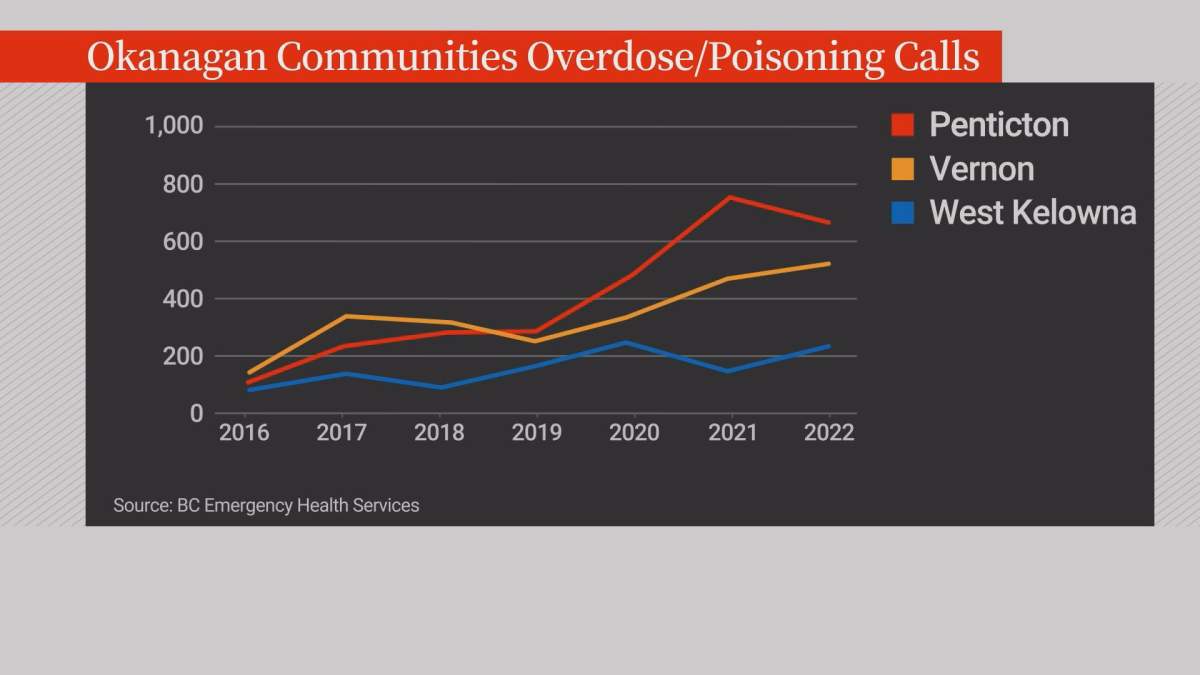
In the Interior, overdose and poisoning calls were up nine percent in 2022 to more than 5,900.
Brian Twaites, a spokesperson for BCEHS, said the data is a sign of the pervasiveness of the toxic drug crisis around the province.
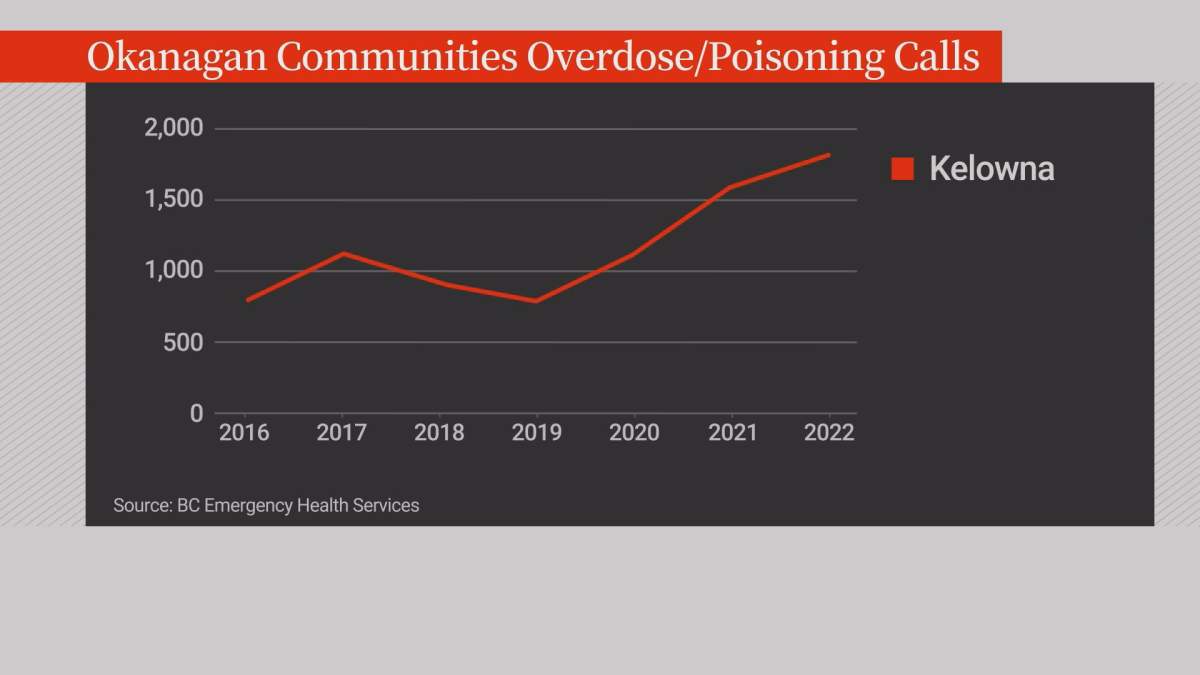
Overdose and drug poising calls also rose in Kelowna to more than 1,800 last year.
It’s the largest annual call volume for the city since the public health emergency was declared in 2016.

Get daily National news
Out of all B.C. communities, Kelowna had the fourth most overdose and poisoning calls in the province last year.
Calls were also up in Vernon (513) and West Kelowna (213) in 2022 but down slightly in Penticton (661).
For Interior Health medical health officer Dr. Carol Fenton, the stats reflect the fact that the drug supply in the Interior and around B.C. continues to be “highly poisonous.”
“We just put out two separate toxic drug alerts yesterday specifically for Cranbrook and Penticton. We know that the street drug supply is toxic across the region,” Fenton said.
Fenton said she couldn’t speculate on why the overdose/poisoning calls are rising in the Interior and dropping in the Vancouver Coastal Health and Fraser Health regions.
However, the medical health officer said tackling the toxic drug crisis is a top priority for Interior Health.
“In the short term, it helps if communities are supportive when we roll out overdose prevention services, which is a reaction to the realities of the toxic drug supply, and in the long term we need to see more policy change like the upcoming decriminalization that is happening in B.C. next week,” Fenton said.
Meanwhile, the president of the union representing paramedics said the ongoing high volume of overdose calls takes a toll.
“We know we do a tough job and we are there to help, but it definitely has an impact on our wellness. There is no question it wears on you,” said Troy Clifford, the president of Ambulance Paramedics and Emergency Dispatchers of B.C.
“Definitely, in many communities, we go to work knowing that we are probably going to see an overdose or multiple overdoses in a shift and that puts a lot of fatigue and stress not only on the paramedics and the first responders but on the families.”
BCEHS acknowledges the overdose crisis is a hard situation to deal with every day and says its critical incident stress program is there to help.
“Quite often a call will get flagged, even before the paramedics make it to the call, that it is a possibility that this may be a high-stress incident and they get contacted by one of their peer debriefers within 24 hours to check in on them to make sure they are doing okay,” said Twaites.
Twaites is urging the public not to use drugs alone and suggests if you do use drugs by yourself, you should use the Lifeguard app.
He said the free phone app allows you to enter your location address and set a timer.
“If you become unresponsive because of a drug poisoning, if you don’t respond to the timer, it will automatically contact our emergency dispatch center and paramedics will get dispatched right away,” Twaites said.
“Fifty-six lives have been saved in British Columbia with the Lifegaurd app.”
BCEHS said the overdose/poisoning data “covers all toxic drugs, which can also include possible poisonings by alcohol or other substances, such as the ingestion of household cleaners.
“However, the data primarily captures toxic illicit drugs.”









Comments
Want to discuss? Please read our Commenting Policy first.