Edmonton researchers are celebrating after a device developed in Alberta that keeps lungs alive between transplant helped 12 patients see successful surgeries.

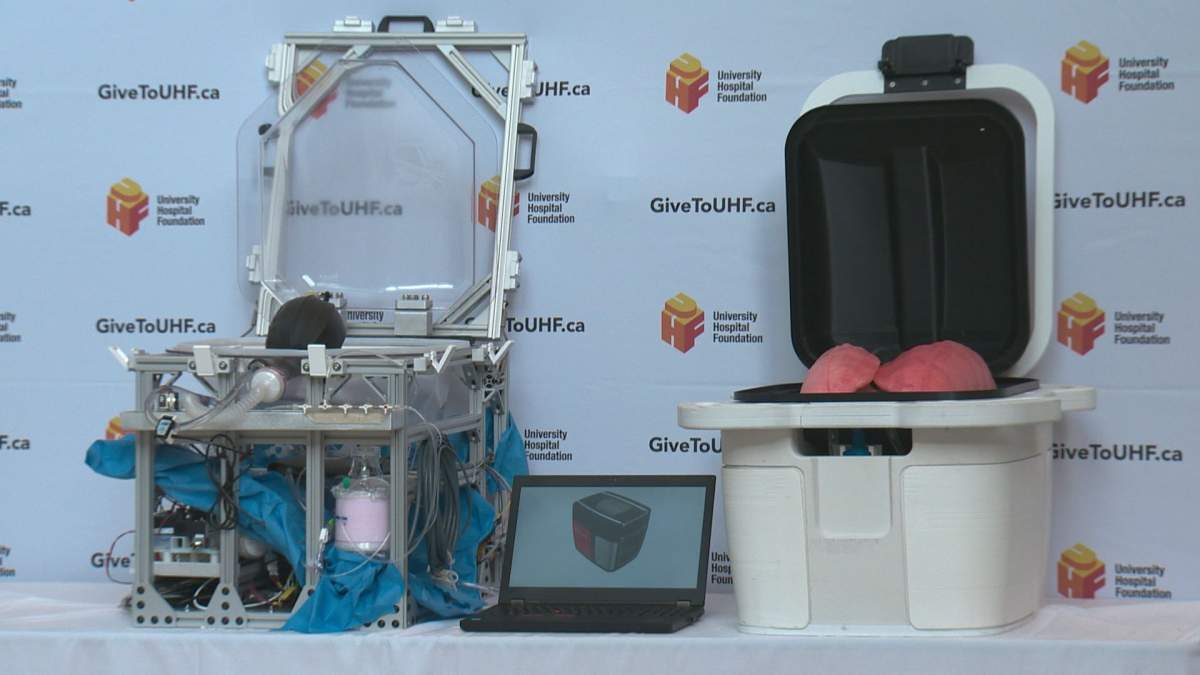
The Ex-Vivo Organ Support System (EVOSS) essentially mimics the human body, using negative pressure that allows the lungs to breathe similarly to how they would in a person.
The device was used in 12 transplants through a clinical trial at the Mazankowski Alberta Heart Institute.
Dr. Darren Freed and Dr. Jayan Nagendran are the two University of Alberta-based researchers who developed it.
“The idea started in my lab,” Freed said. “(We were) looking at the currently available technology, and none of them were really doing what we wanted to do.”
The previous technology that was available used positive pressure, which applied pressurized air to the airway, into the lung, but it could cause damage.
The new device has already helped lungs that would have previously been deemed unusable to be placed in successful transplants after spending some time in the EVOSS machine.

Get weekly health news
“We know that there are many things that happen at the time of donation that may be reversible, if we had the technology to assess them outside of the body,” said Nagendran.
“One of the primary things we can do (with the device), is to breathe for them normally.”
The time in the EVOSS also allows physicians to treat lungs. For example, if lungs were infected with pneumonia, they can then be treated with antibiotics while connected to the machine before transplant.
“They’re (the lungs) put into, for lack of a better word, a robot body,” Nagendran said.
Now, the pair is working with the University Hospital Foundation and Alberta Health Services to further develop the tech, hoping to make it smaller to allow it to replace the cooler-transport method.
“(The current) device… isn’t small enough to take in an ambulance or an airplane, and that’s where we need to take it,” Freed said.
“The smaller we can make it, the more compact it is, the more people will use it.”
Lungs can generally be kept on ice for six to eight hours, but the lung EVOSS device would boost that up to 48 hours.
“They (would) actually replace the ice cooler. They’re the same size, the same weight… we’re not disrupting how things would be transported,” said Nagendran.
“Instead of coming back slowly dying on ice, they (would) come back vibrant and alive, with blood flowing through them and breathing air.”
EVOSS will see a Canadian pilot launch and FDA pivotal clinical trials in 2020.




Comments
Want to discuss? Please read our Commenting Policy first.