On a warm summer morning in June, two men have come to a little trailer in Red Deer, Alta., to inject opioid drugs under the watchful eye of trained medical staff.

John “Max” Malcolm is in good spirits. He jokes with staff and he sits down at one of four cubicles. The other man, who does not share his name, moves to dispose of his used needle. He walks slowly and the nurse on staff stops to check in.
“Are you good?” she asks. The man nods.
Within a few moments, it becomes clear, however, that the man is not okay. A nurse by his side calls for oxygen as the facility’s director asks our Global News cameras to stop filming. The staff begin the life-saving work they’ve done more than 400 times since this site opened last October. The client is given naloxone to reverse the overdose and within just a few moments, his condition improves.
“Good job,” the nurse says as she sits close by. “Keep breathing.”
WATCH: (June 7) Recovering addicts, surviving loved ones call on UCP to restore supervised consumption site funding

The close call has left Malcolm shaken and emotional. He is crying when he agrees to speak to us and apologizes for his tears.
“What just happened always makes me (cry) but no one ever dies here,” he says. “These guys (the staff) are pretty good.”
Malcolm says he has only been using opioid drugs for a few months and he knows he needs to stop.
“I lost a lot of family members, really, in a small amount of time, so my (situation) is extraordinary, but everyone’s is. It’s always something — you’ll never meet anybody in here that has no problems, that doesn’t have a major issue.”
In 2018, Red Deer had the highest rate of apparent drug poisoning deaths related to fentanyl in the province. Forty-seven people were killed.

Get daily National news
Turning Point, a local non-profit outreach agency, worked to set up the temporary overdose prevention site last fall a year ago in a bid to save lives.
READ MORE: Canadian life expectancy has stopped rising because of the opioid crisis
“After a rather difficult weekend, last May actually, where we had, I believe, four fatalities over one weekend. Turning Point kind of declared our own little state of emergency,” said Stacey Carmichael, executive director for Turning Point.
The evidence in support of supervised consumption facilities is growing. According to a recent study from researchers at the BC Centre for disease control, within a 20-month period in B.C., harm reduction measures, including supervised consumption facilities, helped save 3,000 lives.
“What this means is the epidemic could have been up to 2.5 times as high as the one that we actually observed,” said Dr. Michael Irvine, a researcher with the BC Centre for Disease Control and one of the study’s authors.
WATCH: Future of supervised injection sites in jeopardy as funding dries out

Across Canada, however, access to these facilities is varied. At the moment, they only operate in B.C., Alberta, Ontario and Quebec, and some of those provinces are scaling back. In Alberta, funding for any new sites, including a permanent facility planned for Red Deer, was recently frozen, pending a review.
“We just had an election where our government won the largest democratic mandate in Alberta history with an explicit commitment to engage in consultation and an evidence-based review of the social and economic impacts of drug sites before we decide to proceed with any others,” Alberta Premier Jason Kenney said during a recent news conference in Calgary.
In Ontario, three of the province’s 19 sites recently lost provincial funding.
Gillian Kolla, a member of the Overdose Prevention Society, says two Toronto facilities have had to scramble to make alternate arrangements to ensure the doors are kept open.
“We should not have to be fundraising or crowdsourcing to keep an essential health service in the middle of the largest public health crisis of our generation,” said Kolla.
The federal government also stepped in to help, providing facilities like Street Health’s Overdose Prevention Site in Toronto a one-time, six-month funding grant to avoid shutting down.
“The situation that took place in Ontario, we saw that there was few agencies that lost funding … we were able to provide some transitional funding to them,” federal Health Minister Ginette Petitpas Taylor said Thursday during an interview with Global News.
“We recognize that drug harm reduction initiatives work, they save lives and we’re going to continue to follow the situation in Alberta. We’re really pleading with the premier to make sure that they’ll give this matter close attention,” Petitpas Taylor said.
In an emailed statement to Global News, a government of Ontario spokesperson says that under its new funding model, the government expects the number of supervised consumption booths, hours of service and estimated client visits to increase for the 15 approved supervised consumption facilities when compared to the same 15 facilities that were operating under the previous government’s funding model.
“Based on extensive consultation with experts, we are confident that the model we have brought forward is the right approach to connect people struggling with addiction with the care they need and deserve. Applications from interested organizations will continue to be considered on an ongoing basis, based on the outlined criteria,” Hayley Chazen, press secretary for Ontario Health Minister Christine Elliot said in the statement.
READ MORE: Opioid overdose deaths continue to increase in Canada
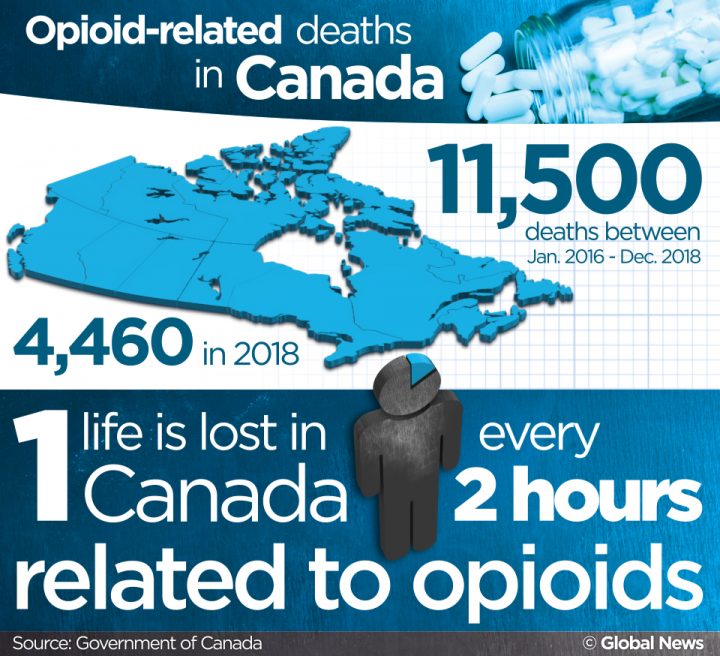
According to numbers released by the federal government Thursday, one life was lost every two hours because of opioids in 2018. Across Canada, 4,460 people died last year, bringing the total number of deaths in Canada to more than 11,500 between January 2016 and December 2018.



Comments