A Massachusetts man has regained his voice after surgeons removed his cancerous larynx and, in a pioneering move, replaced it with a donated one.

Transplants of the so-called voice box are extremely rare and normally aren’t an option for people with active cancer. Marty Kedian is only the third person in the U.S. ever to undergo a total larynx transplant – the others, years ago, because of injuries – and one of a handful reported worldwide.
Surgeons at the Mayo Clinic in Arizona offered Kedian the transplant as part of a new clinical trial aimed at opening the potentially life-changing operation to more patients, including some with cancer, the most common way to lose a larynx.
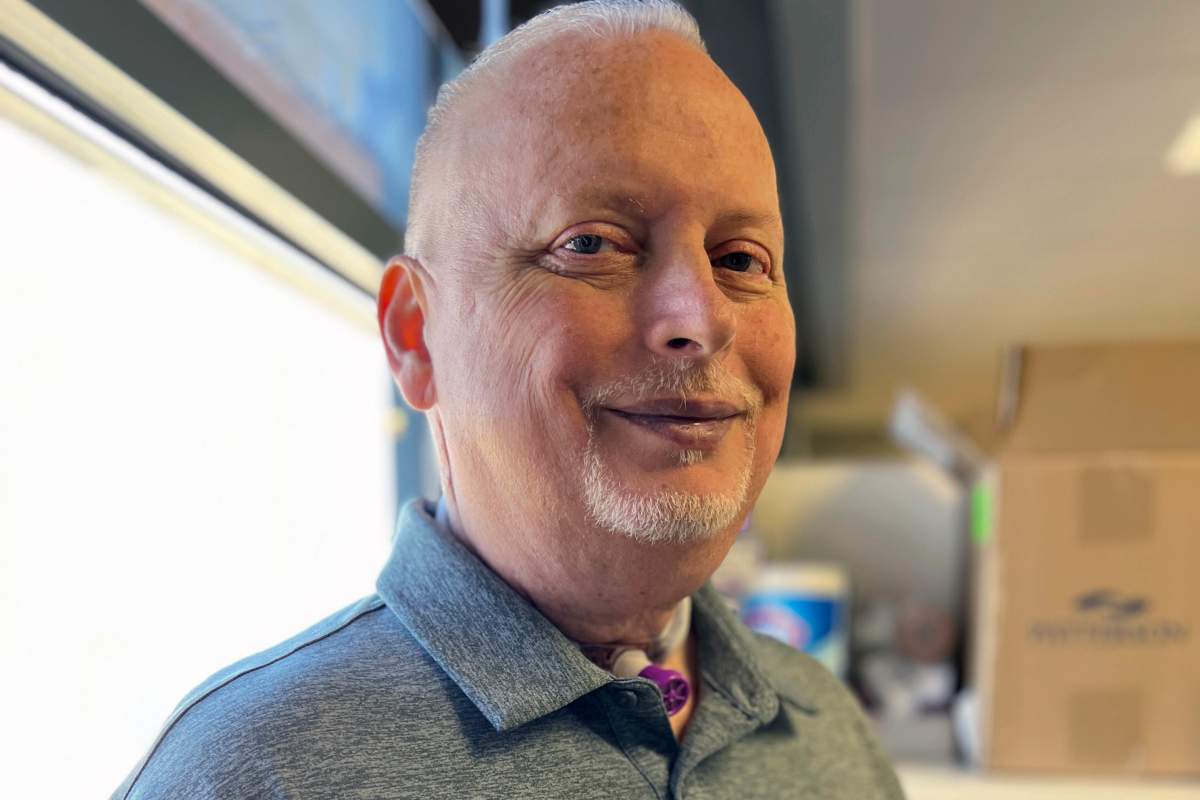
“People need to keep their voice,” Kedian, 59, told The Associated Press four months after his transplant – still hoarse but able to keep up an hourlong conversation. “I want people to know this can be done.”
He became emotional recalling the first time he phoned his 82-year-old mother after the surgery “and she could hear me. … That was important to me, to talk to my mother.”
The study is small — just nine more people will be enrolled. But it may teach scientists best practices for these complex transplants so that one day they could be offered to more people who can’t breathe, swallow or speak on their own because of a damaged or surgically removed larynx.
“Patients become very reclusive, and very kind of walled off from the rest of the world,” said Dr. David Lott, Mayo’s chair of head and neck surgery in Phoenix. He started the study because “my patients tell me, ‘Yeah I may be alive but I’m not really living.’”

Get weekly health news
The larynx may be best known as the voice box but it’s also vital for breathing and swallowing. Muscular tissue flaps called vocal cords open to let air into the lungs, close to prevent food or drink from going the wrong way – and vibrate when air pushes past them to produce speech.
The first two U.S. larynx transplant recipients – at the Cleveland Clinic in 1998 and the University of California, Davis, in 2010 – had lost their voices to injuries, one from a motorcycle accident and the other damaged by a hospital ventilator.
But cancer is the biggest reason. The American Cancer Society estimates more than 12,600 people will be diagnosed with some form of laryngeal cancer this year. While today many undergo voice-preserving treatment, thousands of people have had their larynx completely removed, breathing through what’s called a tracheostomy tube in their neck and struggling to communicate.
Although the earlier U.S. recipients achieved near-normal speech, doctors haven’t embraced these transplants. Partly that’s because people can survive without a larynx – while antirejection drugs that suppress the immune system could spark new or recurring tumors.

“We want to be able to push those boundaries but do it as safely and ethically as we can,” Lott said.
Head-and-neck specialists say the Mayo trial is key to helping larynx transplants become a viable option.
“It isn’t a ‘one-off,’” but an opportunity to finally learn from one patient before operating on the next, said Dr. Marshall Strome, who led the 1998 transplant in Cleveland.
This first attempt in a cancer patient “is the next important step,” he said.
- Head-Smashed-In Buffalo Jump heritage site enjoys boost after shout out on ‘The Pitt’
- What is Nipah virus? What to know about the disease as India faces outbreak
- Pizza Pops contaminated with E. coli tied to 7 hospitalizations, data shows
- Pizza Pops E. coli recall grows as roughly a dozen products now hit
Other options are being studied, noted Dr. Peter Belafsky of UC Davis, who helped perform the 2010 transplant. His patients at high risk of larynx loss record their voice in anticipation of next-generation speech devices that sound like them.
But Belafsky said there’s “still a shot” for larynx transplants to become more common while cautioning it likely will take years more research. One hurdle has been achieving enough nerve regrowth to breathe without a trach tube.
Kedian was diagnosed with a rare laryngeal cartilage cancer about a decade ago. The Haverhill, Massachusetts, man underwent more than a dozen surgeries, eventually needing a trach tube to help him breathe and swallow — and struggled even to muster a raspy whisper through it. He had to retire on disability.
Still, the once gregarious Kedian, known for long conversations with strangers, wouldn’t let doctors remove his entire larynx to cure the cancer. He desperately wanted to read bedtime stories to his granddaughter, with his own voice rather than what he called robotic-sounding speech devices.
Then Kedian’s wife Gina tracked down the Mayo study. Lott decided he was a good candidate because his cancer wasn’t fast-growing and — especially important — Kedian already was taking antirejection drugs for an earlier kidney transplant.
It took 10 months to find a deceased donor with a healthy enough larynx just the right size.
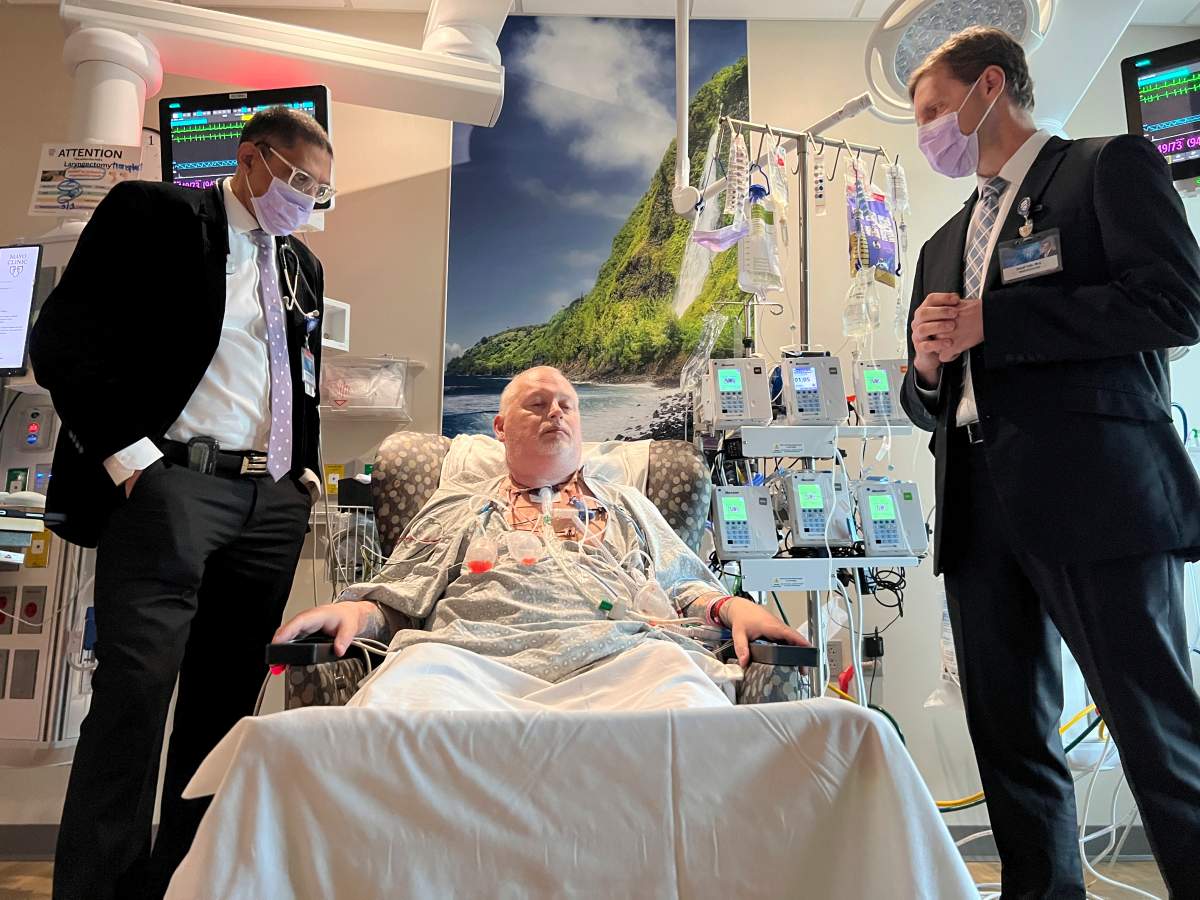
Then on Feb. 29, six surgeons operated for 21 hours. After removing Kedian’s cancerous larynx, they transplanted the donated one plus necessary adjoining tissues – thyroid and parathyroid glands, the pharynx, and the upper part of the trachea – and tiny blood vessels to supply them. Finally, using new microsurgical techniques, they connected nerves critical for Kedian to feel when he needs to swallow and to move the vocal cords.
About three weeks later, Kedian said “Hello.” Soon he’d relearned to swallow, working up from applesauce to macaroni and cheese and hamburgers. He got to say hi to his granddaughter Charlotte via video, part of his homework to just keep talking.
“Every day it’s getting better,” said Kedian, who moves back to Massachusetts soon. His tracheostomy remains in place at least a few more months but “I’m pushing myself to make it go faster because I want these tubes out of me, to go back to a normal life.”
And just as Lott had assured him, Kedian retained his beloved Boston accent.







Comments