It took more than a decade to write. Hundreds of mental health experts contributed to the laborious process. And still, before the first spine has been cracked on the latest iteration of the bible of psychiatry, the new DSM-5 has caused quite a stir.

Critics contend the newest version of the Diagnostic and Statistical Manual of Mental Disorders risks creating diagnosis-creep, with broader definitions that will encompass more people and medicalize things such as normal grieving.
Some have suggested the new reference manual will create false epidemics, with many more children and adults being diagnosed with mental health disorders for which they may be offered powerful drugs.
The Society for Humanistic Psychology is among those complaining about changes in the DSM-5. It argues in particular with the lowering of some diagnostic thresholds, such as the reduction in the number of criteria needed to receive a diagnosis of attention-deficit and hyperactivity disorder (ADHD).
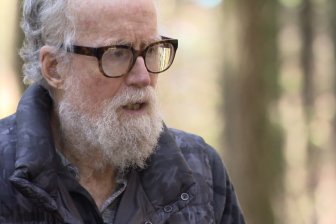
Brent Robbins is president-elect of the Society for Humanistic Psychology and co-chairs the organization’s DSM-5 response committee. Robbins points to the DSM-5’s elimination of what is known as the bereavement exclusion as another place where the new criteria may end up drawing in people who shouldn’t really receive a mental health diagnosis.
In the DSM-IV, a person grieving the death of a loved one could not be diagnosed with major depression in the first two months after that loss. The new manual drops that waiting period, arguing that bereavement can trigger a major depressive episode and people suffering in this way should not have to wait for care.
But Robbins says the change means people coping with normal grief could end up with a diagnosis of major depressive disorder that would stay in their medical records for a lifetime.
“We would essentially take somebody who is going through a normal, transient human experience and say that they have a mental disease,” says Robbins, an associate professor of psychology at Point Park University in Pittsburgh, Penn.
But the physician-in-chief at the Centre for Addiction and Mental Health (CAMH) in Toronto says the claims that psychiatry will draw in multitudes of new cases are unfounded.
“We are not in the business of walking through schools and trying to find a client that we don’t need so that the wait lists at CAMH for child psychiatry go from … three months to now six months or from six months to 12 months,” says Dr. Benoit Mulsant.
Mulsant suggests the aim of the new publication is to right some wrongs in the previous version of the DSM and to help people who are hurting from mental health disorders.
The DSM is produced by the American Psychiatric Association, and will be released by the organization at its annual meeting this weekend in San Francisco.
This is the first full revision of the manual since the DSM-IV was released in 1994. Much has been learned in that time and the new edition will reflect the evolving science. And yet, something that hasn’t changed is perhaps at the root of much of the arguing that has gone on about the new reference manual.
Unlike cancer or diabetes, which can be confirmed by studying the results of a biopsy or the readings of a blood test, mental health disorders are still diagnosed by symptoms.
There is no blood test that can distinguish transient attacks of the blues from depression, no imaging technology that differentiates normal high-spiritedness from ADHD. And though science is trying to find physiological roots for mental health disorders, progress has been slower than many in the field hoped and expected.
Mulsant says that when the DSM-III was written in 1980, experts were convinced that biology-based tests for mental health disorders were not far off.
“(And) if you had asked me when we did No. 4, we really thought that was the last one being like that and that by No. 5 we’d have biologically based diagnostic classifications,” he says.
And yet that’s still not the case.
So over the past 14 years, more than 400 international researchers have worked on the scientific studies that were undertaken to revise those parts of the DSM that were deemed in need of updating, said Dr. Dilip Jeste, APA president.
There were white papers. There were 13 working groups set up to tackle different aspects of the job and 13 scientific conferences held. There were field trials conducted to see if revised diagnoses would have the desired effect – identify the people who needed help without drawing in more who did not. There were public consultation periods.
“DSM-5 is the product of the most extensive discussion and debate – as part of a transparent process – of any DSM,” Jeste said in written responses to questions.
He thinks it’s natural that a project like this would draw a lot of criticism.
“Mental disorders affect people’s lives in real and meaningful ways,” Jeste says. “It is understandable that patients and their loved ones would feel impassioned about ensuring that people with mental disorders are diagnosed correctly and receive appropriate treatment.”
So what are the changes? A number relate to where a disorder sits among other like disorders, or what a condition is called.
For instance, hoarding is no longer considered a symptom of obsessive-compulsive disorder; it is now a disorder on its own. Conversely, the term Asperger’s syndrome is being dropped in favour of autism spectrum disorder, which encompasses high-functioning and low-functioning people with autism. That is a move that incited a lot of discontent.
Mental retardation is being dropped, having been deemed to be too offensive a term. The new diagnosis is “intellectual disability” and, unlike mental retardation, it is not simply IQ based.
The diagnosis will use a definition that assesses adaptive living skills as well as cognitive abilities, says Dr. Susan Swedo, who led the DSM-5 neurodevelopmental disorders working group. Swedo is the chief of the pediatrics and developmental neuroscience branch at the U.S. National Institute of Mental Health.
She’s sorry to see the term mental retardation go because it stated quite clearly what the condition was. “(But) it became socially unacceptable.”
In a twist that illustrates the complexity of crafting these diagnoses and hitting upon the right language for them, a group called the Voice of the Retarded actually lobbied Swedo’s working group to retain the diagnosis of mental retardation. They felt society should drop the stigma surrounding the word retardation, not lose the term.
But Swedo said the term had been dropped from legislation in the U.S. and elsewhere, and it was felt there was no going back.
The APA won’t say precisely how many diagnoses the DSM-5 will contain, saying the aim was to try to keep this edition of the manual to roughly the same length as the DSM-IV, which included 283 diagnoses over 943 pages.


Comments