New Brunswicker Nicole Daigle got COVID-19 back in January, amid the Omicron wave.

At first, symptoms were like that of the common cold, but the illness progressed to what she described as the sickest three weeks of her life.
“After three weeks, the symptoms actually started to subside,” she said in an interview Friday. “But that’s when things did take a turn for the worse, a real turn, and I lost the COVID symptoms … but I started gaining really concerning symptoms.”
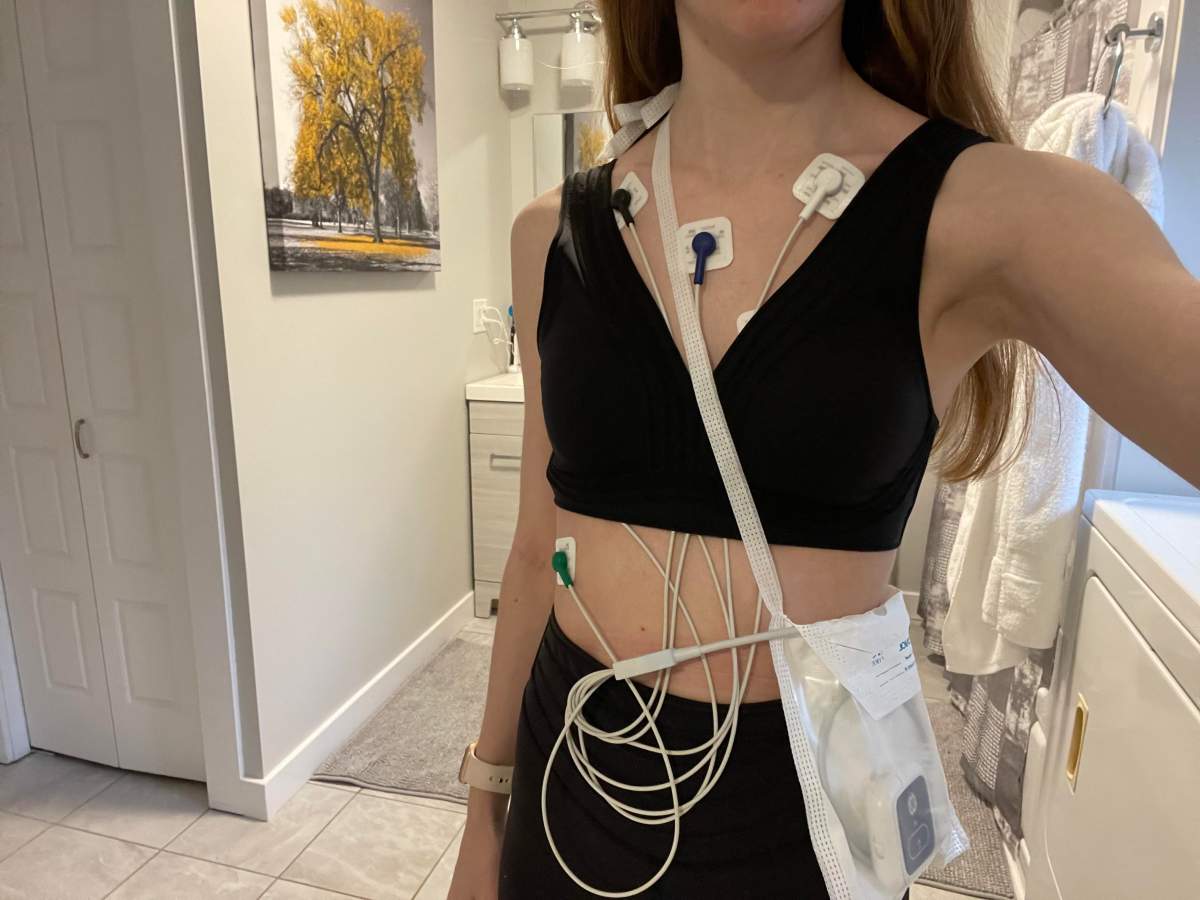
She started having chest pain, shortness of breath, migraines, brain fog, issues with her memory, and an erratic heart rate.
“I would be afraid to shower because I was afraid I was going to pass out,” she said.
Daigle was experiencing heart rates of 140 beats per minute while she was seated and relaxed on the couch. Her regular doctor told her to go to the emergency department in Fredericton.
“The first few times, they really didn’t know what to do with me,” she said. “They kind of thought it was unrelated. So at first I was asked questions like ‘are you really anxious?’ and ‘is there stress going on in your life?’“
Daigle had been fully vaccinated with two doses at the time of her infection.
Doctors were almost insistent her symptoms were related to anxiety and gave her a medication called Ativan to calm her down, but she said it made her feel sedated and didn’t actually help her heart rate issues.

Get weekly health news
Following almost seven visits to the ER, once by ambulance, she said she was told she had post-COVID-19 disorder – otherwise known as long COVID.
She was referred to a cardiologist who would give her two more diagnoses connected to her COVID-19 infection.
Daigle was diagnosed with postural orthostatic tachycardia syndrome and inappropriate sinus tachycardia.
It explained much of her symptoms, she said. She now is taking heart medication and physiotherapy and sees light at the end of the tunnel she’s been walking through for more than five months.
But generally, the experience left her frustrated.
“It was a lot of advocating for myself and saying this is serious,” she said. “There was definitely a lot of frustration of saying you know this is serious and it kind of felt like at the time it was being treated as case-by-case basis.”
Daigle worries about those who may not have the strength to speak up for themselves in the situation she found herself in.
She said she hopes sharing her story will help inform people and help them find their voice in a system that has much to learn about the impact, onset and treatment of long COVID.

But Daigle isn’t alone in her experience with long COVID.
Ability New Brunswick, a non-profit that helps people with disabilities and mobility issues, said it is seeing more and more referrals to them due to long COVID.
“People dealing with symptoms and difficulties such as neurological conditions, mobility conditions as a result of long COVID – it’s something we’re needing to turn our mind to,” said it’s executive director Haley Flaro.
She said the organization has to adjust despite limited research and resources available for long COVID and those experiencing it.
“In our organization, what we’re concerned about, is navigating disability services and supports,” she said in an interview Friday. “Long COVID isn’t recognized as a disability right now because it is new.”
Flaro said there are lot of questions about how it impacts people who need to take time off work, whether those with long COVID qualify for sick benefits, or disability.
“That’s top of mind,” she said.
For her, it is about ensuring no one falls through the cracks while the medical community learns more about long COVID and it’s impacts.
“It’s going to be something Ability New Brunswick is going to have to be loud about so we don’t leave this population behind.”













Comments
Want to discuss? Please read our Commenting Policy first.