WASHINGTON — Gene editing is getting fresh attention thanks to a successful lab experiment with human embryos. But for all the angst over possibly altering reproduction years from now, this technology already is used by scientists every day in fields ranging from agriculture to drug development.

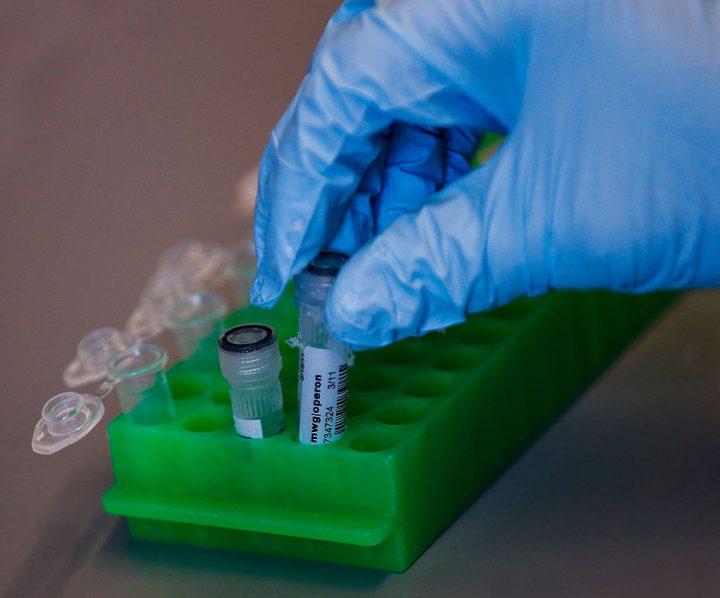
New gene editing tools let scientists alter the DNA of living cells — from plants, animals, even humans — more precisely than ever before. Think of it as a biological cut-and-paste program. A look at the science.
READ MORE: Scientists are pushing to genetically modify babies to avoid diseases
What is gene editing
While scientists have long been able to find defective genes, fixing them has been so cumbersome that it’s slowed development of genetic therapies. There are several gene editing methods, but a tool called CRISPR-Cas9 has sparked a boom in research as laboratories worldwide adopted it over the past five years because it’s faster, cheaper, simple to use with minimal training and allows manipulation of multiple genes at the same time.
How it works
Pieces of RNA are engineered to be a guide that homes in on the targeted stretch of genetic material. The Cas9 is an enzyme that acts like molecular scissors to snip that spot. That allows scientists to delete, repair, or replace a particular gene.
READ MORE: Scientists, ethicists tackle gene-editing ethics
Medical research
The fresh attention comes from research involving human embryos. In laboratory experiments, a team lead by Oregon researchers used CRISPR to successfully repair a heart-damaging gene in human embryos, marking a step toward one day being able to prevent inherited diseases from being passed on to the next generation. But there’s wide agreement that more research is needed before ever testing the technique in pregnancy.

Get breaking National news
The biggest everyday use of CRISPR so far is to engineer animals with human-like disorders for basic research, such as learning how genes cause disease or influence development and what therapies might help.
WATCH: Mother implanted with 18-year-old embryo gives birth to 2nd child

But promising research, in labs and animals so far, also suggests gene editing might lead to treatments for such diseases as sickle cell, cancer, maybe Huntington’s — by altering cells and returning them to the body. Another project aims to one day grow transplantable human organs inside pigs.
The biggest hurdle
Safety is a key question because gene editing isn’t always precise enough; there’s the possibility of accidentally cutting DNA that’s similar to the real target. Researchers have improved precision in recent years, but out-of-body treatments like using cells as drugs get around the fear of fixing one problem only to spark another.
The ethics controversy
Altering genes in sperm, eggs or embryos can spread those changes to future generations, so-called “germline” engineering. But it’s ethically charged because future generations couldn’t consent, any long-term negative effects might not become apparent for years, and there’s concern about babies designed with enhanced traits rather than to prevent disease.
READ MORE: Health Canada approves sale of genetically modified salmon for human consumption
Earlier this year, an ethics report from the prestigious National Academy of Sciences opened the door to lab research to figure out how to make such changes — but said if germline editing ever is allowed, it should be reserved for serious diseases with no good alternatives and performed under rigorous oversight.
Is the legal?
Where you live determines if, or what kind of, research can be performed on human embryos. Some countries, especially in Europe, ban germline research. Britain allows basic lab research only.
In the U.S., scientists can perform laboratory embryo research only with private, not federal taxpayer, funding, as the Oregon team did. Any attempt to study germline editing in pregnant women would require permission from the Food and Drug Administration, which is currently prohibited by Congress from reviewing any such request.
WATCH: Baby born in China after spending 13 years as a frozen embryo

Beyond medicine
Researchers also are using gene editing to hatch malaria-resistant mosquitoes, grow strains of algae that produce biofuels, improve crop growth, even make mushrooms that don’t brown as quickly.
This Associated Press series was produced in partnership with the Howard Hughes Medical Institute’s Department of Science Education. The AP is solely responsible for all content.






Comments
Want to discuss? Please read our Commenting Policy first.