This is the latest article in a Global News investigation into fertility in Canada, and the emotional and financial impact infertility has on Canadians struggling to conceive.

***
Sexually-transmitted infections can wreak havoc on future child-bearing plans — and your child’s life — if you’re not careful.
The biggest fertility-killing culprit is a serious complication that can arise if a bacterial STI like gonorrhea or chlamydia is left untreated. It’s called pelvic inflammatory disease (PID) and both men and women can get it.
Women, though, are believed to be most at risk.
“Essentially the infection ravages the pelvis,” said Toronto fertility doctor Marjorie Dixon. “I see it all the time, sadly.”
PID prevalence
It develops in 10 to 15 per cent of women with untreated chlamydia, according to University of Toronto epidemiologist Dionne Gesink. What’s perhaps most concerning is that you may not even realize you have it.
Up to 70 per cent of women and 50 per cent of men have no symptoms of chlamydia after infection. Most women infected with gonorrhea are also asymptomatic. So the consequences of PID may not be felt until it’s too late.
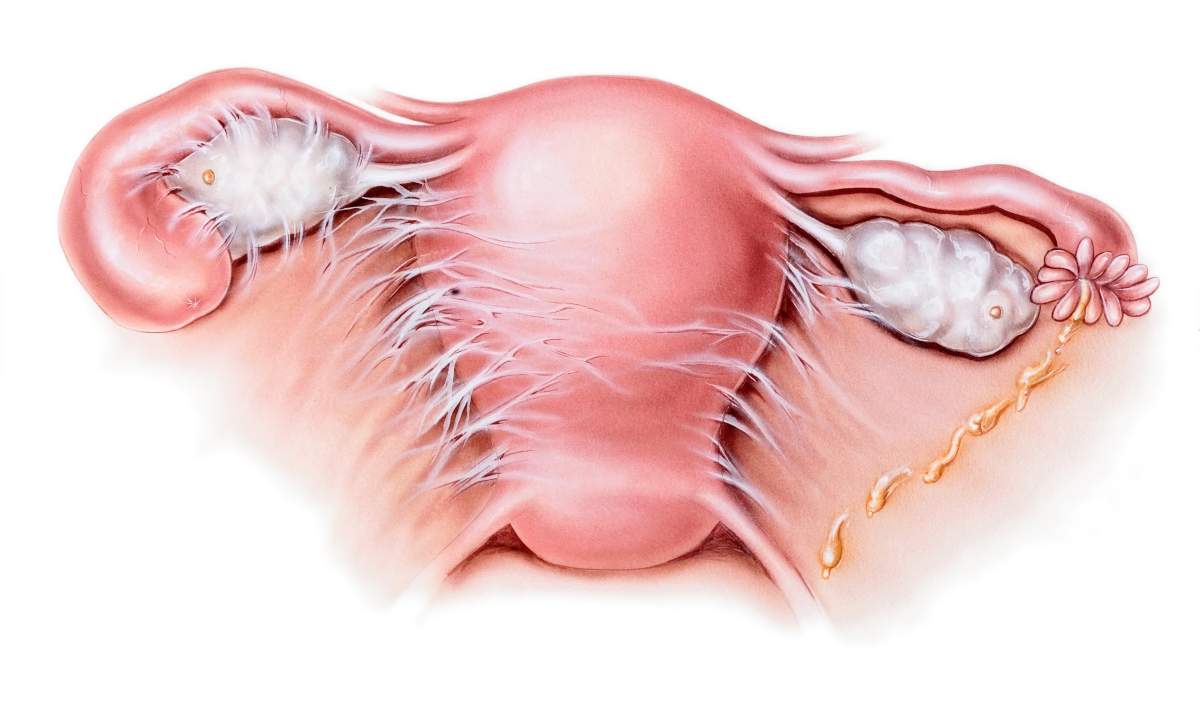
“‘Silent’ PID may cause the most damage, including permanent damage, to the Fallopian tubes and uterus, which can lead to infertility.”
One in eight (12 per cent of) women who have a history of PID will have trouble getting pregnant, Gesink says. They’re also at greater risk of an ectopic pregnancy, which is when the fetus develops outside the uterus.
Five per cent of the total population of women have PID, Gesink adds. However it’s hard to say what percentage of them have it from a previous bout of chlamydia or gonorrhea because there are a number of other ailments that can cause PID including: non-STI bacterial infections like bacterial vaginosis, endometriosis, and intrauterine devices (IUDs).
Gesink says IUD problems “are usually limited to the first three weeks after insertion.”
WATCH: Health Canada reviewing safety of birth control implant as women join class-action lawsuit

“PID is definitely an issue.”
How does PID cause damage?

Get weekly health news
Gesink explains PID causes the pelvis to swell and pushes organs together. As they touch, a sticky web is formed that in the Fallopian tubes that will block sperm from reaching the egg.
“You can think of it like a little kid playing with gum in your hands. The gum sticks to both sides of your hands and when you pull your hands apart and get this web.”
Even after the PID is treated and the swelling goes down, the “gumming” remains.
Getting treatment for it won’t reverse the damage to one’s pelvic anatomy — it just stops the damage from getting worse, according to Gesink. Surgery to clear up the blocked tubes might help, however Gesink warns it can sometimes create scarring that leaves its own blockage.
‘PID for men’
In men, Gesink says, chlamydia or gonorrhea can cause chronic inflammation of the urethra which is “like PID but for men.”
It can reportedly cause the urethra to narrow and limit sperm flow. In some cases it can also creep its way up the urethra into the epididymis (a tube behind the testes that stores and carries sperm) leading to inflammation of the epididymis called epididymitis which is “also like PID for men.”
Symptoms
PID has similar symptoms to how chlamydia and gonorrhea can manifest itself in both men and women.
According to the Centers for Disease Control and Prevention, the STIs are sometimes accompanied by an unusual discharge and pain during urination (and, to a lesser degree for men, pain or swelling in the testes).
The STIs can be transmitted rectally and orally too. In the case of the latter, “essentially you get the infection in your throat,” according to Gesink.
READ MORE: Men are driving Ontario’s rising gonorrhea rate, data shows
Women with PID symptoms may experience fever as well as pain or bleeding during sex as well. They may also see spotting between periods.
When testing for PID, the Mayo Clinic explains a doctor would order a urine test and/or do a swab for STIs, as well as potentially perform a pelvic exam.
So how can you prevent it?
The length of time it takes for gonorrhea or chlamydia to turn into PID depends on the person, Gesink says.
“Some women can develop PID within a matter of days.”
READ MORE: Drug-resistant STIs mean ‘if you don’t wrap it up, you’re in trouble’
The sooner a STI is treated, the less chance there is for PID to develop and for extensive damage to occur.
There’s one other easy way to avoid this whole ordeal.
“Tell the men to wear rubber booties,” Dixon said. “Always, always, always.”



Comments