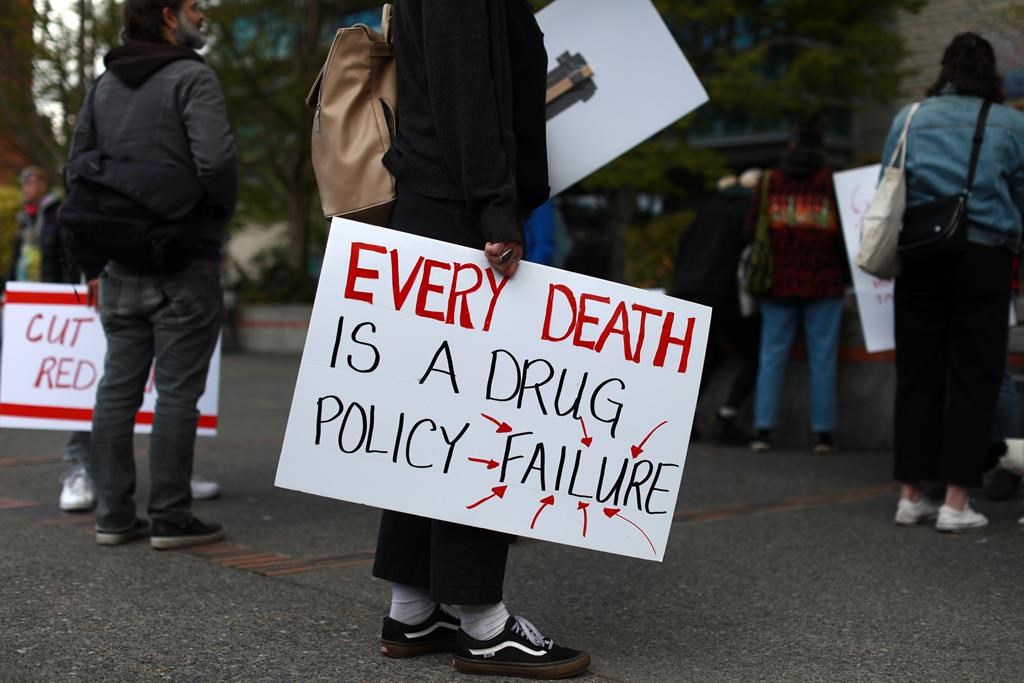
Advocates in the Simcoe Muskoka region are calling for more action to address toxic drug poisoning in the Simcoe Muskoka area.

The report released by the Canadian Drug Policy Coalition calls for swift actions to address the drug poisoning crisis in Barrie and highlights what advocates say is a need for decriminalization.
The report comes from a two-day community dialogue in Barrie called Getting to Tomorrow: Ending the Overdose Crisis in October 2021, held in partnership between the John Howard Society Simcoe and Muskoka, Indigenous Harm Reduction Network, and the Gilbert Centre.
The agencies involved brought together people with lived experiences, harm reduction staff, city officials, and Indigenous people to look at how to move forward.
“We are focused on empowering people who use drugs to participate in the decisions that impact their lives, which includes paying people a fair wage for the work they do. More than anyone else, people who use drugs know what will help address the toxic drug crisis,” said Sarah Tilley of the Gilbert Centre.
“We need to make sure that people who share their knowledge aren’t putting themselves at greater risk of criminal scrutiny. We must continue to advocate for decriminalization at a federal level.”
She said the issue is emphasized by the fact that several people with lived experiences involved in the study have since passed away from reasons directly or indirectly related to drug use.

Get weekly health news
Preliminary data from the Simcoe Muskoka District Health Unit shows that there were 111 confirmed and probable opioid-related deaths in Simcoe Muskoka in the first 10 months of 2022, which was 21 per cent lower than the 151 deaths in the first 10 months of 2021, but is still substantially higher than what was observed before the pandemic (2017-2019), both locally and across the province.
The report outlines five key things that need to be changed to address the crisis, including creating and finding a task force of people with lived experiences, requesting a city-wide exemption in Barrie to decriminalize drugs, and increasing access to affordable housing. The other two recommendations are training protocols in human rights and more collaboration in policy development.
The health unit found that From January to June of 2022, there were approximately 40 opioid poisoning emergency department visits per month among Simcoe Muskoka residents.
“Opioid poisoning emergency department visits rates in Simcoe Muskoka have nearly quadrupled when compared to what was observed between 2010 and 2014 and are more than five times higher compared to the rates between 2004 and 2008,” the health unit said in a statement.
The Simcoe Muskoka rates have been significantly higher than the comparable provincial rates since 2004, the health unit found.
Tilley said it is challenging to maintain a safe supply of drugs without regulation and with criminalization.
She said this issue goes beyond those society views as the typical drug user, noting that it is becoming an increasing problem in the construction trade for workers who get injured to treat their pain.
“This is a class issue, and this is a racial issue, and it’s often difficult to find those specific numbers, but when people are not able to access conventional streams of support, that’s often when they’re turned away, and the folks that are most likely to be turned away from conventional forms of support largely in this community as well, are Indigenous and people of colour,” Tilley said.







Comments